Airborne Contamination Insights From the Pandemic and Strategies to Optimize Efficiency
By Jennifer Wagner, PhD, CIC, and Damon G. Greeley, PE, CEM, HFDP, CBCP, EDAC, CHFM, A-IPC
As more people are vaccinated against the COVID-19 virus, many would like to resume their routine medical appointments and elective surgeries. Research indicates that airborne transmission of aerosolized droplets may be a significant factor for the spread of the SARS-CoV-2 coronavirus. As a result, hospitals and healthcare providers must understand the impact of airborne transmission pathways in different healthcare environments to provide a safe environment for their patients.
A hospital is like a “mini city.” There are multiple types of spaces such as patient rooms, exam rooms, procedure rooms, ORs, café/dining areas, waiting rooms, and offices—each with their own requirements for airflow rates and exchanges to ensure safe “turnover” times between use.
Multiple variables can impact transmission of SARS-CoV-2 or any airborne pathogen. Below are insights, strategies, key challenges, and potential solutions for ensuring enhanced air quality in healthcare environments.
Insights regarding aerosolized droplets
There are several insights regarding aerosolized droplets:
Speed of travel. Aerosolized droplets can spread very quickly. Research published in the Proceedings of the National Academy of Sciences, the official journal of the National Academy of Sciences, found that highly sensitive laser light scattering observations revealed that loud speech can emit thousands of oral fluid droplets per second. According to the study, louder speech produces even more droplets. Just one minute of loud speaking can generate almost 1,000 virus-containing droplets that stay in the air for more than eight minutes. This impacts considerations for airflow introduction into a specific space and the design of the exhaust air system.
Length of time. Aerosolized droplets also remain viable for extended periods. Researchers with the National Institute of Allergy and Infectious Diseases’ Laboratory of Virology in the Division of Intramural Research in Hamilton, Montana, used a nebulizer to blow coronaviruses into the air. They found that infectious viruses could remain in the air for up to three hours, according to study results published in the New England Journal of Medicine. This reinforces the importance of air exchange rates and the introduction of fresh air into healthcare environments, especially rooms that host aerosol-generating procedures.
Travel distance. Finally, aerosolized droplets can travel farther than you might think. While the universal standard is 6 feet, are you at risk if the space is larger? In a study published in the journal Physics of Fluids and using computational fluid dynamics simulation, researchers with the Defense and Security Research Institute at the University of Nicosia in Greece found that aerosolized droplets could travel up to 18 feet in as little as five seconds. Humidity, temperature, and airflow (both velocity and direction) can all impact droplet travel distance, which emphasizes the importance of airflow testing in healthcare environments.
Air quality improvement approaches
There are several approaches to improving air quality:
Molecular aggregating. As a result of the pandemic, multiple vendors have developed technologies that introduce charged molecules into healthcare spaces with the goal of aggregating the smaller aerosolized droplets and particles for easier capture by an HVAC system filter. However, this technology runs the risk of concentrating the airborne microbes into an infectious dose before the microbes are drawn away from the occupant breathing zone.
Air filters. Many healthcare organizations wish to improve their air filtration systems as a result of the pandemic. ASHRAE recommends the use of filters with a rating of MERV 13 (or higher) within mechanical systems to capture and reduce the risk of aerosol spread. Consider testing and documenting the capacity of the entire facility’s air handling system before installing upgraded filters, as pressure from higher-rated filters might overwork the system and reduce airflow, causing air stagnation in certain spaces.
High-efficiency filtration approaches. Aerosolized droplets carrying the virus can be 1–5 micrometers large. High-efficiency particulate air (HEPA) filters are able to capture 99.97% of particles 0.3 micrometers or smaller. Permanent or portable HEPA fan filter units can be placed in immediate areas of high use and are most effective in smaller enclosed areas. If a systemwide HEPA filter is installed, there is no need for added ultraviolet light systems, as once the aerosol is captured it is no longer viable. One of the downsides of an air filtration approach is that the system fan must run continuously to remove air particulates; when the heat or air conditioning is not on, the system does not do anything to clean the air. And, if the filter is turned off, particulates can fall from the filter.
Increased frequency vs. increased amount. Increasing the frequency of air exchanges can reduce the potential spread of the virus by exhausting potentially contaminated air and aerosols in a space, replacing that with clean filtered air. Increasing the amount of outside air (OA) helps reduce the risk of airborne transmission of the virus by diluting potentially contaminated inside air with OA.
How airflow mapping can improve operational efficiency
As hospitals wish to return to pre-pandemic levels for elective surgeries, the safety of both patients and healthcare workers is top of mind for healthcare leaders. Because the coronavirus is an airborne pathogen, it is critically important to understand the airflow within different healthcare environments. Since air is invisible, an alternate method is needed for visualizing how the air transports particles within a given space to reduce the risk of airborne infections.
The AirStatEQI™ Airflow Visualization Device provides real-time airflow visualization data. This hand-held technology allows the user to input space identification information, room temperature, and specific humidity. It measures the velocity and direction of the air at various points within a given space, and using a contamination risk mapping algorithm, the device quickly produces a risk map with color-coded areas: green (in compliance), yellow (below target levels), and red (critical).
Each reading (two to 10 per room) takes approximately 20 seconds, minimizing disruption to patient care. The risk readings can be uploaded to an interactive floor plan that includes key elements (surgical table, back tables, anesthesia station, case carts) and stores data from each reading, enabling analytics and trending of historical conditions. This data can be used to improve airflow and safety and optimize procedure and exam room scheduling.
A hospital in the Midwest recently used the AirStatEQI to substantially reduce their hospital-acquired infection (HAI) rate in their OR suite. One physician’s HAI rate began to spike. Specializing in knee replacement surgery, the physician was assigned a dedicated operating room. Using the AirStatEQI in conjunction with its proprietary algorithm, the hospital discovered the root cause of airflow cross-contamination, allowing the hospital to make changes to the ventilation locations and rates that resulted in a significantly reduced infection rate.
Figure 1: OR Risk Before and After
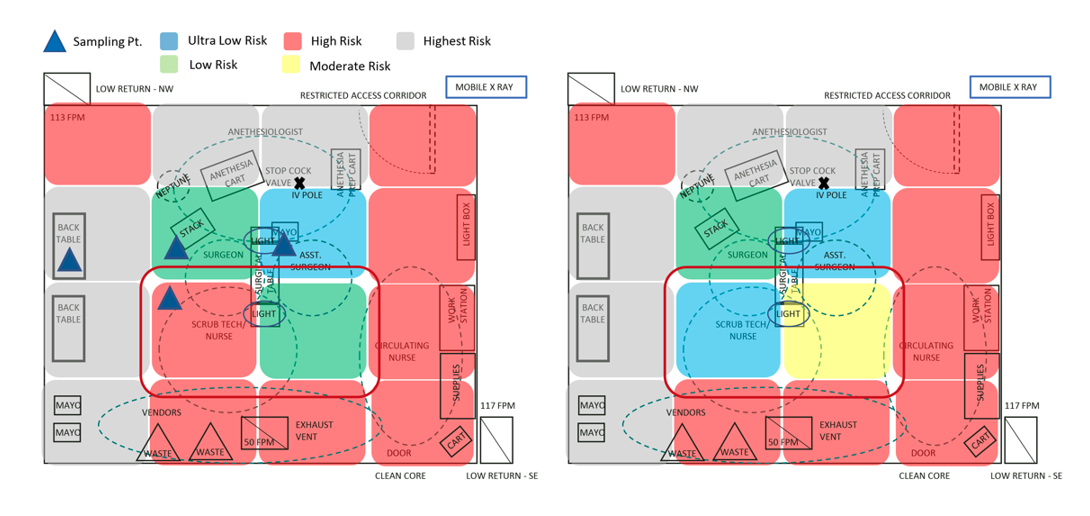
Source: OnSite-LLC
Validation that healthcare environments are safe and functioning optimally is a critical element of restoring consumer and employee confidence in healthcare providers. Accurate data and analysis can provide the much-needed evidence that these environments are safe for both patients and healthcare workers.
Jennifer Wagner, PhD, CIC, is managing partner with OnSite-LLC in northern California. She can be reached at jwagner@onsite-llc.com. Damon G. Greeley, PE, CEM, HFDP, CBCP, EDAC, CHFM, A-IPC, is managing partner with OnSite-LLC in Indianapolis, Indiana. He can be reached at dgreeley@onsite-llc.com.
