Adaptable Expertise
Implementing Transition and Operations Planning in the Face of a Pandemic
By Teri Joy, RN, BSN, CEN, TCRN, EDAC
Challenges + context
As a result of the COVID-19 pandemic, many hospital design and construction projects were placed on hold while healthcare organizations addressed surge capacity issues. As hospitals anticipate a return to pre-pandemic operations, healthcare leaders seek to complete these projects as quickly and efficiently as possible, recognizing that a move into a new facility or renovated space provides an opportunity to assess patient care models, staffing levels, and workflow—and provides, in some instances, better infection control and cleaner environments.

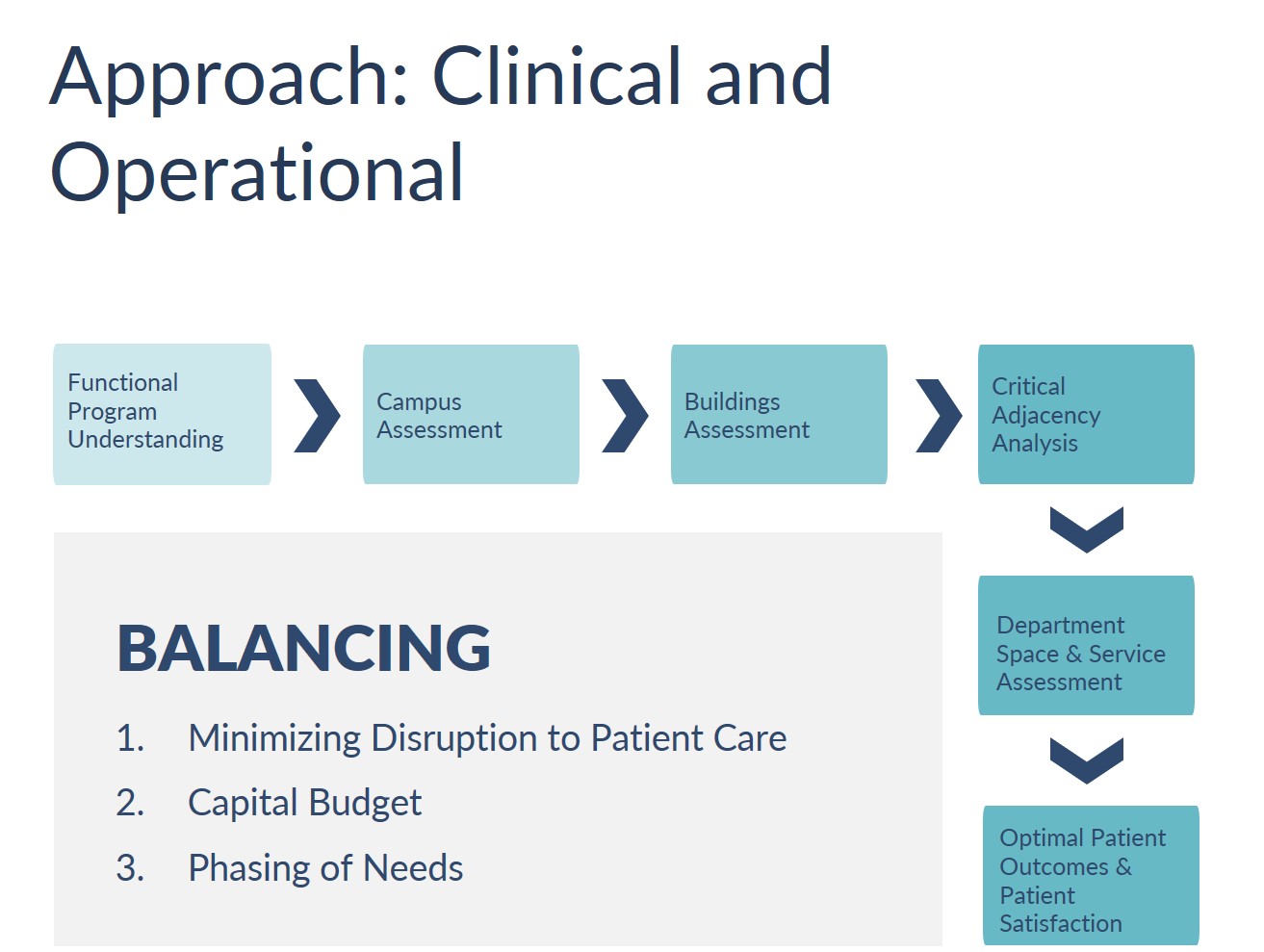
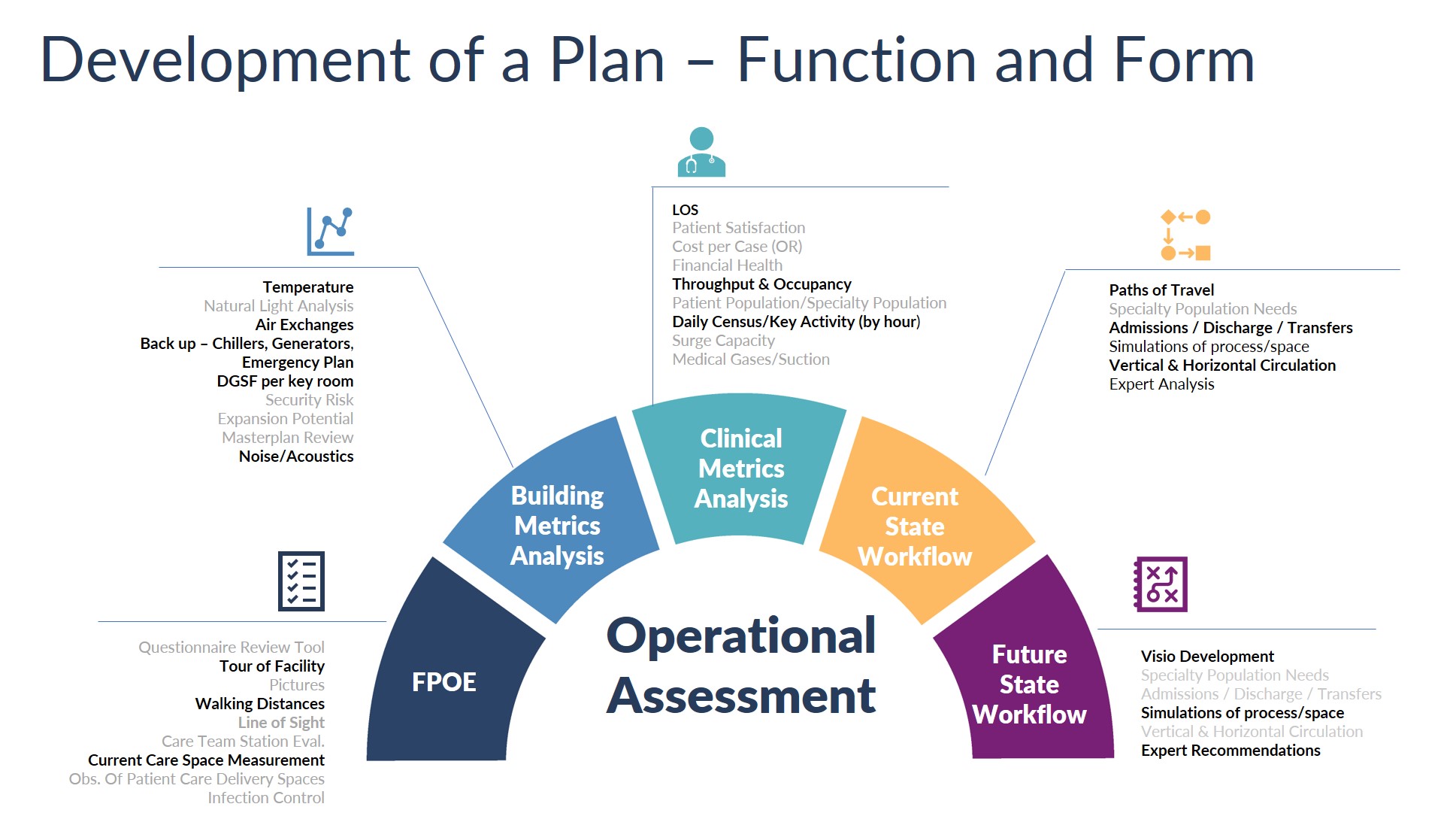
Focus on desired functions and outcomes. The goal in operations planning is to design a space that supports the desired function and allows future flexibility for patient care, including treatment surges. Preparation for the unexpected—such as a global pandemic or natural disaster—and consideration of the facility hazard vulnerability analysis are key elements of the planning and transition processes. An understanding of CMS/Joint Commission requirements for environment of care conditions is also important when planning a healthcare environment. Operational planners use evidence-based design principles and analyze the current state, future goals, and regulatory considerations.
Transition planning provides hospital staff and frontline caregivers with an understanding of how the new building or space will support patient care patterns. When coupled with robust operations planning, the process can help healthcare leaders maximize operational efficiency in a shorter period. The building and environment can also support performance metrics to enable continuous improvement.
Often, a single clinical planner or team member will handle transition planning as well as operations planning. Both are critical for the implementation of broad organizational changes and commissioning of new spaces. How effectively the transition is executed can have a major impact on the success of the new space or facility. As such, meticulous planning—such as an operational planning assessment by an experienced clinical planner—is key to optimization. Below are additional suggestions for navigating the transition planning and operations planning processes.
Transparency + consistency
Prepare through schematics. Preparation is vital for a successful transition planning project. During the pandemic, clinicians and clinical planners functioned with information that changed daily, while critical analysis of potential care processes was more crucial than ever. One of the keys in optimization of transition planning is to include operations planning in the schematic design phase to better understand the workflows that will occur in the new space. Today’s operations planning must ensure flexibility of any new space to accommodate surge plans, respiratory patients, PPE, and sequestered units with their own airflow requirements. The clinical operations planner also ensures that regulatory requirements and strategic functional operational goals related to the functional program are preserved. This knowledge base and skill set can be applied in surge and unplanned urgent situations to provide optimal solutions and allow hospital staff to focus on patient care.
Once a preliminary operational plan exists, it should be validated with clinicians and key facility experts, including security and infection control personnel, IT, EVS, and supply chain representatives, to ensure ideal use of space in the future. This discussion, led by a seasoned clinical operations planner, can help define the paths of travel for standard workflows during the design phase to optimize efficiencies, care delivery, and throughput. This ensures that the seven Lean flows of healthcare are addressed in the early phase of the project. The plan that results from this discussion should be part of the hospital emergency response plan. Planning should discuss and identify alternate care sites and flexible care areas, plus considerations for infection control. This leads to a clear knowledge of the building’s capabilities, enabling hospital leaders to make quick and well-informed care decisions in high-intensity circumstances.
In one example project, the design team was working with a team from the organization to decrease costs. The initial design removed hallway sinks throughout the facility. The operations planner presented evidence that showed this was not ideal from an infection control or flexibility standpoint, and the team was able to make a change. This example illustrates how early operations planning, which emphasizes function and outcomes, can enhance the success of a project and make transition planning intuitive and efficient, placing the focus on processes, flexibility, and change.
Priority + flexibility
The ability to quickly set priorities and the flexibility to respond to a deluge of changing circumstances are vitally important during a planned or unplanned event.
Protocols shape priorities—and vice versa. Operations planning is a balancing act when considering protocols in the new facility. It is critical for the design team to understand the nature of design requests made by the clinical staff. In some instances, bedside clinicians make suggestions based on their current situation rather than incorporating or considering the future state. Experienced planners can help the design team understand the bedside clinicians’ wishes while incorporating best practices, disaster response, and optimal efficiencies into the ideal future state. Designing with, instead of for, the healthcare team is an important step in functional design.
Observe the existing operation. One useful technique to understand the current design is a functional post-occupancy evaluation of the client’s current space, which reveals insights into the daily operations in the environment as well as any challenges staff members routinely face. This also helps planners identify which environmental features staff and patients favor, and which design features offload a healthcare provider’s physical and cognitive burdens to the built environment. Getting feedback from the people who use the space every day is one of the best ways to ensure design functionality for daily use. The environment should intuitively promote best practice based on layout and design. For example, a sink should be close to a room’s door or the first step in an entry sequence into the room that promotes a behavior such as hand hygiene.
Expect expectations to evolve. When the proposed design does not match with the organizational goals for the future, a savvy operations planner can facilitate conversations with the clinical team to reconcile current needs in practice and expectations. Expectations often evolve as new priorities are identified, necessitating a flexible and nimble plan that can evolve as well. The operations planner can provide effective analysis and communication with the design team early in the project, enabling flexibility, financial savings, and optimal clinical design features for the end users.
Communicate to collaborate. Communication is central to getting everyone on the same page for a true collaborative effort. It is essential for the design team, end users, and administrative decision-makers to understand what is happening in the healthcare environment, the rationale for each action, and why key decisions are important. Transparency in planning builds trust between the design team and administrators, end users, and patients, resulting in an evidence-based design that supports all users and customers.
In one example, the team analyzed paths of travel for a new design that included limited connections to support services in a second tower. The operations planner mapped out various travel paths for normal activities as well as emergency situations and conducted a case study presentation with key stakeholders. The availability of adequate quantitative data allowed the administrative owner along with the end users to define goals and set priorities for the project.
Emerging COVID-19 considerations. A clinical planner can add value in a robust or quick analysis of how to leverage space in an unplanned situation. The pandemic called for quick analysis of an unknown disease and functions in a built environment to keep patients and staff safe. For example, many hospitals wanted to separate sick and healthy patients at various entrances and throughout the hospital. In times of crisis, expedited analysis from a deeply knowledgeable operational planner can speed the implementation of safe, cost-effective solutions for adapting the built environment to care for patients with infectious diseases. Their expertise can be applied to the healthcare environment as units are converted to special disease units, such as has happened with COVID-19 units. The operational planners can collaborate with engineers to determine airflow capabilities and other physical needs of this patient population. Their deep understanding of clinical workflows, the seven Lean flows in healthcare, and the needs of patients and staff make an operational planner a key resource for adaptable care in a crisis.
Key categories operational planners use to review COVID-19 adaptations to buildings and workflow
Key drivers that have emerged through the pandemic are causing growth in the industry centered around adaptability and the prioritization of patient safety and comfort. As we’ve seen with COVID-19, when case counts surge and cause rapid change in space and functional needs, the ability to adapt and persevere in an unknown environment is critical. While these traits are abundant among healthcare teams, design teams aim to facilitate clinicians’ efforts by providing adaptable spaces that can support a shifting care delivery model.
Another set of drivers: the importance of communication and the ability to interact with loved ones even while in isolation. With a new disease, fear and uncertainty rise among patients, especially when the risk of transmission means that family members are restricted from access. Remote visitation comes with physical and logistical challenges, including access to video and the time staff are required to spend communicating with remote family members. Design teams seek to create environments that make socially distanced communication easier for staff via whiteboards outside patient rooms, video monitors for communication from a distance, and virtual access for family and other support persons.
Decision-making + transparency
Structure frames decisions and outcomes. Operations planners can help determine the organization’s needs and set up a proven and consistent structure for communication and oversight from the beginning of the project or crisis. Keeping a detailed decision log over the course of the event/project helps illustrate best practices and predict how the future state can deliver on project goals and support all regulatory functions in the healthcare environment. Awareness of regulatory guidelines, including FGI, Joint Commission, CMS, and OSHA, informs the design in conjunction with building functionality to optimize patient care. The same is true in an acute disaster/surge situation. The data and metrics generated from past and current regulatory surveys and findings also help the project team understand specific design change needs, lessons learned, and options for flexible spaces within the healthcare environment.
Organized communication enables transparency. An effective operations planner uses this information to educate the design team and owners, facilitating the necessary transparency for team buy-in. Operations planners have organizational and communications skills that can unify the design and healthcare teams to foster a shared vision. Modeling good communication and identification of interdependencies between design, MEP, and clinical teams early in the project will avoid the pitfall of team members functioning in silos as the project moves forward. Transparency provides team members with the rationale for major decisions to achieve alignment and constructive, respectful conversations and to ensure that everyone feels part of the team. Clinical operational planners often take on the role of educator for design and clinical teams, combining rationale, costs, and real-world experience into effective and creative building solutions.
Metrics + emotional intelligence
Metrics make for better decisions. To aid in decision-making during transitions and accommodate the different ways each healthcare leader visualizes the process, it helps to have clear baseline facility metrics. Any time you have a full understanding of the current state, adaptations for future change are more informed. An established starting point saves time in future state reviews/adaptations. Collecting this data involves analysis and research that will streamline the process of delivering the information to executives, whose schedules often do not include much time for reviewing documents. Presenting the data clearly is the quickest path to the baseline information needed for operations and the most expedient approach for busy professionals who must review the numbers, ask questions, and make decisions.
Balance micro and macro perspectives. It can sometimes be difficult for leaders to see things the way an end user sees them. An operational planner can bridge the gap as a translator. For leaders, seeing the project data summarized neatly in one location with the important metrics highlighted helps bring focus to critical decisions and harness the energy needed to complete the project. Operations planners focus the discussion on key issues that illuminate potential future challenges and allow for preemptive diagnosis and correction before they result in major cost impacts. They can help the design team understand why some design elements are more beneficial than others, thanks to their insight that comes from engagement with multiple healthcare clients, end users, and executive decision-makers. That clinical expertise makes a difference in a building’s design and, ultimately, its function. The operational planner can provide end users and administrative teams a bridge between best practice and return on investment.
Operations planning: Critical to success
Building trust across stakeholders allows for rapid change. An experienced and especially savvy operations planner can bring not just clinical expertise to the table, but also a high level of emotional intelligence. Authenticity and integrity allow clinical planners to understand the concerns of key stakeholders—both administrative decision-makers and end users. An effective operations planner can assess the organization’s current state of readiness and knowledge and quickly gauge whether the chosen approach is working and how to course correct if necessary. Demonstrating empathy for people and their processes establishes strong working relationships built on trust that allow the entire design team to navigate difficult decisions. This thoughtful, honest approach is effective when rapid decision-making is needed.
Emotional intelligence involves connecting with users and administrators on a personal level. This is a skill learned during a nursing career, when dealing with many people each day, and it can be potently harnessed in healthcare design. It’s important to understand how a project directly impacts each person and their work. Displaying this knowledge in decision-making contributes to the goal of making each person’s work meaningful and reinforcing that the organization cares about its people, not just about completing the project. This approach greatly helps end users adopt new ideas and processes with comfort.
Planning for a higher purpose. Many healthcare providers view their career as a higher calling, a service, and a gift to be used to help people. Because of this, changes to their environments can evoke strong emotions that can be challenging for designers and architects to address. An operations planner with a clinical background can mitigate those challenges by modeling understanding, empathy, and connectedness to support the shared goal of safe patient care. This approach unites the team and provides a supportive environment for difficult decision-making and significant change. Most people who work in healthcare derive meaning and satisfaction from it. Together, a team can create meaningful work environments that can be effective and healing spaces for all users.
Teri Joy is senior healthcare operations planner with BSA LifeStructures. Joy also serves as a NIHD Board Member. She can be reached at 317-617-5732 or tjoy@bsalifestructures.com.