A Team Approach to Fall Prevention
March/April 2013
![]()
A Team Approach to Fall Prevention

The Falls Team on 5 South, Hunterdon Medical Center. (l to r) Cindy Winchock, Cathy Edmonds, Kristy Alfano, Yvonne Kunz, Michele Betz, Pamela Abraham, and Michelle Tirado.
Falls are a growing health concern, especially within the acute care arena. A fall is defined as “an event which results in a person coming to rest inadvertently on the ground or floor or other lower level” (Johnson et al., 2011). More than 30% of adults age 65 and older fall each year (Centers for Disease Control and Prevention, 2011), and up to 50% of adults age 85 and older fall each year (Bohl et al., 2010). With the aging population, the incidence of falls is only expected to increase.
Patient falls are the most common patient safety issue in hospitals, accounting for up to 32% of reported patient safety incidents (Ramos Vieira et al., 2011). About one-third of patients who fall suffer physical harm, including death (Ramos Vieira et al., 2011). Among hospitalized patients, rates of falls range from 1.97 to 8.40 falls per 1,000 patient-days (Leep Hunderfund et al., 2011). Approximately 30% of inpatient falls lead to physical injury, and 6% result in serious injury (Stenberg & Wann Hansoon, 2011). In 2008, the Centers for Medicare and Medicaid stopped reimbursing for hospital-acquired conditions that should never occur during hospitalization (Shever et al., 2011). A fall is considered one of these “never events” because there is a sufficient evidence base to prevent falls (Shever et al., 2011).
Falls prolong hospitalization and increase cost of care (Leep Hunderfund et al., 2011). In 2010, the cost of falls to the healthcare system nationwide was estimated to be $28.2 billion (Centers for Disease Control and Prevention, 2011). The cost of falls is expected to reach more than $54 billion by 2020 (Centers for Disease Control and Prevention, 2011). Lack of reminbursement for these costly events is a major motivating factor for hospitals to ensure that patients receive evidence-based care to prevent inpatient falls (Shever et al., 2011).
In addition to increased costs, falls result in many injuries: fear of further falls, loss of independence, social isolation, loss of mobility, muscle weakness, postural hypotension, and depression (Capezuti et al., 2008; Ramos Vieira et al., 2011). Falls in the hospital also affect direct-care staff, who may experience guilt and apprehension (Kalisch et al., 2012).
Hunterdon Medical Center in Flemington, New Jersey, is not unique in its quest to decrease the number of in-patient falls. However, the staff has created some unique interventions to bring about awareness and prevention of falls. The nursing staff of the Intermediate Care Unit was especially concerned about preventing falls following one such “never event.” A fairly healthy, elderly gentleman had been sitting at the edge of his bed eating lunch when he leaned on the bedside table to stand. Unfortunately, the man fell forward, sustaining injuries to his face and neck. Despite prompt care and surgery, the patient succumbed to his injuries and passed away a few days after the fall. The staff decided to delve into the available evidence, asking themselves, “Could this fall have been prevented? What risk factors did this patient have? What should we have done differently?” And most importantly, “How can we make sure this never happens to another one of our patients?”
Risk Factors and Assessment
Multiple intrinsic risk factors have been identified for falls. These include advanced age, muscle weakness, gait or balance problems, visual impairment, altered bowel or bladder elimination patterns, dizziness or vertigo, depression, cognitive deficits, impaired activities of daily living, use of psychotropic medications, and a history of falls (Leep Hunderfund et al., 2011). Risk factors for falls in the acute care setting include these intrinsic risk factors in addition to extrinsic risk factors: use of bed rails, toileting needs, improper bed height, type of floor surface, unfamiliar environment, clutter in the room, medical equipment in the room, and poor lighting (Ramos Vieira et al., 2011). Assessing and modifying the patient’s environment has been shown to be an effective way to decrease falls (Shever et al., 2011).
Several risk assessment scales or tools exist to address intrinsic and extrinsic risk factors. These tools aim to quantify a patient’s fall risk based on the sum of multiple risk factors so that a patient is “at risk for falling” when their score reaches a certain number. According to a survey of 140 nurse managers, the most commonly used assessment tool is the Morse Fall Risk Assessment Tool, with 40% of nurse managers stating that their facility uses this tool (Shever et al., 2011). The frequency of assessment varies among facilities, but generally a patient is assessed for fall risk on admission and once per shift.
Falls precautions should be initiated on patients who are identified as a fall risk by whichever assessment tool is used. Falls precautions in the literature include bed alarms, frequent rounding or hourly rounds, safety sitters, relocating patients closer to nursing stations, signs identifying at-risk patients, low bed position, wristband alerts, lowering the side rails on the bed, physical restraints, increased monitoring or surveillance, call-light within reach, nonskid socks, pharmacy referrals, physical therapy, personal items within reach, and increased ambulation (Shever et al., 2011).
Hunterdon Medical Center started using the Morse Fall Risk Assessment Tool in October of 2011, when the hospital switched computerized charting systems. Prior to that, the hospital had used a tool that was developed by the hospital. The interventions reflected in the falls precautions policy have remained the same despite the change in assessment tool used. If a patient is assessed to be at risk for falls, a “red dot” sticker is applied to the patient’s name band, a red dot sticker is placed on their chart, and a larger red dot sign is placed on the patient’s door. Bed and chair alarms are to be used as well.
Despite having an effective falls prevention policy, the rates of patient falls remained high on the Intermediate Care Unit. According to the National Database of Nursing Quality Indicators, the rate of falls on that unit per 1,000 patient days was 3.45 for 2009, and 5.07 for the first quarter of 2010, above the mean for Magnet hospitals of 3.26 and 3.19, respectively. During discussion at a unit-based staff meeting, several staff members voiced interest in forming a sub-committee in an effort to decrease the number of falls, especially in light of the catastrophic fall that had occurred on the unit. The sub-committee became the Falls Team and included the clinical nurse leader of the unit, staff nurses, patient care assistants, and the unit director.
Falls Team Pilot Implementation
The pilot unit for the implementation of the Falls Team was a 29-bed Intermediate Care Unit, 5 South. This unit is a telemetry step-down unit that typically cares for cardiac and neurologic diagnoses, such as stroke, altered mental status, chest pain, atrial fibrillation/flutter, post-myocardial infarction, and pre- and post-cath lab procedures. The unit also receives overflow patients when necessary. Nurses generally have a 4:1 or 5:1 ratio during the day shift and a 5:1 or 6:1 ratio during the night shift. Patient care assistants care for an average of 8 to 12 patients during the day shift and 10 to 14 patients during the night shift.
The Falls Team first met in March 2010 and began by reviewing the incident reports of the 28 falls that occurred in 2009. The team identified that despite the existence of an effective falls prevention protocol, 18 of the falls, or 64%, were preventable falls. These falls were considered preventable because bed or chair monitors were not alarmed, beds were left in the high position, patients at risk to fall were far from the nursing station, but mostly due to patients being left alone for toileting purposes. The Falls Team then performed a mandatory staff in-service to reinforce the falls precautions protocol. The new unit policy went into effect, which states that staff members would stay within sight of patients when in the bathroom or on the commode in an effort to prevent toileting falls.
The Falls Team’s findings—that toileting falls led to the majority of the preventable falls on the unit—is supported in the literature as well. An estimated 40% of inpatient falls are related to toileting (Jones et al., 201).
The Falls Team also designed and performed audits to ensure that the appropriate falls precautions were being utilized for patients assessed to be at risk to fall. The team members continue to audit the use of bed and chair alarms, beds in low position, and red dot signage on the door and wristbands for at-risk patients.
The Team created “Don’t Fall, Call” posters for the patient rooms. These posters are positioned across from each bed to be visible to patients and families. Team members also created an educational flier about falls precautions and placed that in the welcome binder on every bedside table. Patients and families are educated about safety, including bed and chair alarms, and the red dot protocol.
The most innovative intervention that resulted from the Falls Team meetings is a Falls Bulletin. This bulletin describes the unique circumstances that led to each fall in an effort to prevent future falls stemming from similar situations. The bulletin is written after each fall by one of the staff nurses on the Falls Team, and describes the “who, what, where, and why” of the fall without using patient identifiers. For example, the first bulletin was sent out after a patient fell in the bathroom getting dressed for discharge home. The patient was unharmed during the fall and was in fact discharged that day, but the bulletin lead to a great discussion at a staff meeting about when the falls protocol should be terminated: the moment discharge orders are written or when the patient is safely in the car to be driven home? The consensus of the staff after this fall was that falls precautions would be in place until the patient has physically left the hospital, and practice has adapted to accordingly.
The bulletin is disseminated to every staff member’s mailbox and includes a section for feedback or suggestions at the bottom of the bulletin. Any feedback or suggestions that come back to the Falls Team are discussed at the next staff meeting. The idea of the bulletin has been adopted throughout the hospital as a way of alerting all staff of a patient fall.
Since the start of the Falls Team, the unit’s message board has a section for “days without a fall.” This board also states what the goal is (100 days without a fall) and whether or not the last fall was preventable or unpreventable. This way, every staff member knows when the last fall occurred and how close to the “goal date” the unit is. The unit director encourages celebratory luncheons when a goal is achieved.
The final intervention that came from the Falls Team was a reorganization of chair alarm equipment. Chair monitor sets include a chair pad, monitor set-up, and a cord that attaches directly into the call-light. Prior to the Falls Team, it was difficult to find a complete chair monitor set. The team reorganized the equipment so that all the pads are in one bin, the monitors are in one bin, and the cords are in another bin. Additional chair alarms were purchased to increase availability, so that there would be an alarm for every patient chair. This decreases the hunting and gathering and increases the likelihood that a chair monitor will be used, and the chair alarm audits reflect an increase in usage.
Results
The Falls Team has been shown to be an effective way to foster awareness and prevention of inpatient falls. 5 South had 28 falls in 2009, and 10 in the first quarter of 2010 prior to the implementation of the Falls Team. As mentioned previously, the average rate of falls per 1,000 patient days in 2009 was 3.45, and 5.07 in the first quarter of 2010. After the implementation of the Falls Team in March 2010, the falls rate dropped to 1.96, 1.52, and 2.52 for the second, third, and fourth quarters of 2010, respectively. The number of falls for 2010 was 23, including the 10 in the first quarter. In 2011, the total number of falls on 5 South was 10, a dramatic decrease from 28 two years prior (Figure 1). This equates to a decrease of 65%. The average rate per 1,000 patients for 2011 was 1.40 (Figure 2).
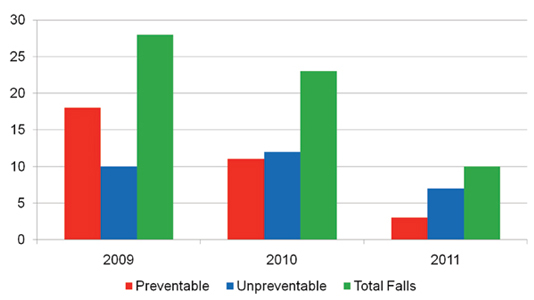
Figure 1. Falls on 5 South
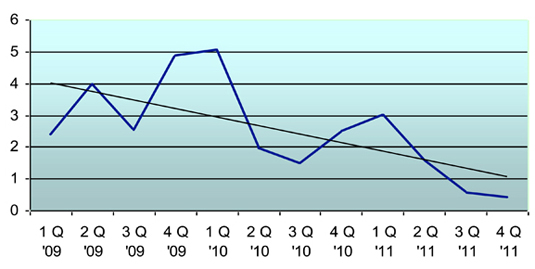
Figure 2. Rate of Falls per 1,000 Patient Days on 5 South
The unit also went more than 100 days without a fall, which had never occurred before on 5 South. The staff celebrated that not only was there a decrease in the number of falls, but there was a shift in the type of falls with the majority now being unpreventable. Unpreventable falls are defined by 5 South staff as falls that occur despite all preventive measures being in place. Preventive measures include bed/chair monitors, visible signage that denotes risk to fall, staff answering alarms promptly, staying with the patient during toileting, and appropriate staffing. On the other hand, preventable falls occur when staff deems they could have done more to prevent a fall. These falls occur due to forgotten bed or chair alarms, alarms that are set too quietly or not sensitive enough, leaving a patient alone during toileting, understaffing, not answering alarms promptly, and not initiating falls precautions on a patient that actually is at-risk to fall.
As stated before, preventable falls accounted for 64% of the total number of falls in 2009. In 2011, preventable falls accounted for 30% of the total number of falls. Simply looking at preventable falls, the staff of 5 South was able to decrease the number of these events by 15 in the course of 2 years. Preventing 15 falls, at an average of $20,000 per fall, means a potential cost avoidance of $300,000. Cost aside, the other “injuries” caused by falls are prevented: social isolation, fear of falling, and physical and mental decline. Money is the biggest “seller” of the Falls Team, but nursing, being the art of caring, certainly values increased quality of life and decreased patient suffering more than any dollar amount.
Implications for Practice
Since the success of the Falls Team on 5 South, the idea of a falls team as well as many of the interventions have gone hospital-wide. The other medical units have created falls teams and have adapted their own versions of the Falls Bulletin. The bulletins have been largely accepted hospital-wide as a great way to communicate among the staff. The “Don’t Fall, Call” signs have also been adopted by the other units.
5 South has also held collaborative meetings with physical therapy, since early ambulation is one of the aforementioned methods to prevent inpatient falls. The clinical nurse leaders on the unit work closely with home care, as well, to facilitate transitions into home physical therapy for appropriate patients. Geriatric rounds also take place on the unit, which facilitates referrals for physical therapy, home care, Lifeline, more appropriate medication regimes, and outpatient social services in an effort to promote safety across the continuum of care.
The Falls Team continues to meet monthly in an effort to sustain the initial success. Future goals of the team are to create a “Mobility Program” in conjunction with physical therapy, to determine safe exercises that can be done in the hospital and home that maintain muscle mass and balance. The Falls Team is only the beginning in a culture of change to promote safety, well being, and quality of care for the patients of Hunterdon Medical Center as well as the staff.
Catherine Edmonds is a clinical nurse leader at Hunterdon Medical Center in Flemington, New Jersey. She may be contacted at Edmonds.Catherine@hunterdonhealthcare.org.
References
Acknowledgments
The author would like to acknowledge the support of the nursing administration of Hunterdon Medical Center and to extend special thanks to the members of the 5 South Falls Team:
Pamela Abraham, MSN, RN, CNL
Michele Betz, RN, Chair of Team
Michelle Tirado, MSN
Cindy Winchock, RN
Yvonne Kunz, BSN, RN
Jessica Karroll, RN
Stacey VanAuken, PCA
Denise Mateyka, PCA
Kristy Alfano, BSN, Director of the Intermediate Care Unit
Thanks, too, to all of the staff of 5 South for their hard work and dedication to decreasing the number of inpatient falls.
