MRI Safety 10 Years Later
November / December 2011
![]()
MRI Safety 10 Years Later
What can we learn from the accident that killed Michael Colombini?
In the summer of 2001, the radiology world was shocked to learn of an accident at Westchester Medical Center in New York state in which 6-year-old Michael Colombini was killed while being prepared for an MRI exam. Sedated and positioned in the scanner, the child’s oxygen saturation levels began dropping quickly. After the piped-in oxygen serving the MRI scanner room malfunctioned, the anesthesiologist attending the child called for oxygen. A nurse, who was not part of the MRI department staff, responded to the anesthesiologist’s calls and, meeting the anesthesiologist at the door to the MRI scanner room, handed him a steel oxygen tank. When the oxygen tank was brought into the MRI scanner room, the profound magnetic strength of the MRI scanner drew it out of the anesthesiologist’s hands and into the scanner, where it struck and killed the young boy.
 Nearly all practitioners who have some responsibility for safety in MRI—risk managers, technologists, compliance officers, administrators, patient safety officers, and radiologists—are aware of this most infamous MRI accident: the 2001 death of Michael Colombini. Ten years after this tragedy, it is appropriate to measure what we know about it, how that knowledge has reshaped MRI safety, and how improvements in MRI safety measure up.
Nearly all practitioners who have some responsibility for safety in MRI—risk managers, technologists, compliance officers, administrators, patient safety officers, and radiologists—are aware of this most infamous MRI accident: the 2001 death of Michael Colombini. Ten years after this tragedy, it is appropriate to measure what we know about it, how that knowledge has reshaped MRI safety, and how improvements in MRI safety measure up.
When we speak about MRI safety to medical professionals at conferences, we sometimes ask members of the audience what they know about the Colombini tragedy. Typically they can recount only three or four superficial facts about the accident:
- The accident involved an oxygen cylinder drawn into the MRI scanner.
- The oxygen cylinder struck and killed the boy, who was in the MRI scanner.
- The oxygen cylinder was introduced to the MRI suite by a nurse or anesthesiologist.
- The hospital where this occurred is located in New York.
Sadly, the patent truth in each of these statements might equip each of us for a trivia contest but does not help us to understand—and more importantly, prevent—adverse events such as the Colombini accident. Too often, the industry focuses on capriciously selected “symptomatic” details and not on true root causes involving systemic deficiencies that impact our decision-making.
Beyond the Symptoms
It deserves to be said that it is often very difficult to glean “lessons learned” from medical errors that wind up in litigation or are otherwise subject to strict confidentiality. While that is frequently the case, it is not so with the Colombini civil litigation.
Following Michael Colombini’s death in 2001, civil suits were filed and litigation proceeded until a settlement was reached near the end of 2009. As part of the settlement, none of the parties will comment on the accident or the litigation, though none of the parties sought to have the legal records of the incident sealed.
In 2010, after the last of the civil suit documents were filed with the Westchester County Clerk’s Office, we were able to undertake a comprehensive assessment. And while we know that there were discoveries, depositions, and affidavits collected during the civil litigation that were not filed with the court (and therefore not accessible as a part of the public record on this incident), sufficient first-person depositions, reports, and accounts of the events of the day and those leading up to it are in the record to paint a reasonably complete picture.
When looking in detail at the chronology of events that transpired, we can see past the symptoms and into the systemic issues that played a major role in allowing this incident to occur:
Westchester Medical Center (WMC) owned a purpose-built MRI suite addition to the hospital and the single MRI scanner within. The hospital subcontracted the management and operation of the MRI service to University Imaging Medical Associates (UIMA), which employed the MRI clinical and technical staff. UIMA’s president was also the chair of radiology for WMC.
Well prior to the accident, lines of authority and responsibility among the UIMA employees and between the on-site employees and either UIMA or WMC management were unclear, at best. Employees of UIMA were unclear which organization they worked for or which supervisors had responsibility for safety issues.
The MRI technologists at UIMA were neither required to have—nor were they offered—any MRI safety training as a part of their duties. While there were a couple of perfunctory paragraphs about MRI safety in the policy and procedure manual, the technologist charged with administering the Colombini exam was unaware that any facility policy and procedure manual even existed.
Both MRI technologists on duty at the time of the accident had been employed at UIMA for about 6 months prior to the accident. Neither UIMA’s radiologists nor senior administration had offices on-site at the MRI facility.
The anesthesiologist who sedated the young boy on the day of the accident was unknown to both of the technologists, and he had not received any MRI safety training from either WMC or UIMA. His familiarity with the UIMA MRI facilities, policies, and procedures was simply presumed by the technologists, who did not ask.
During preparation for the MRI, Michael was given sedative several times in an attempt to calm him for the exam. After Michael was placed in the MRI scanner but preceding the beginning of the exam, the anesthesiologist observed the boy’s oxygen saturation levels falling. Upon checking the output rate of the piped-in oxygen at the wall outlet, the anesthesiologist observed that no oxygen was flowing.
The MRI technologist (#1) who was to have administered the exam came to the MRI scanner room door, which the anesthesiologist had opened to speak with her. After speaking with the anesthesiologist, the technologist sought out her colleague, technologist #2, who was preparing films from a prior examination. She informed him that there was a problem with the oxygen supply to the MRI patient, and asked if he could investigate the stand-alone bulk oxygen cylinders in the MRI computer equipment room that fed the wall outlets in the MRI scanner room.
MRI technologist #2 stated that he would show her how to check and/or change out the bulk cylinder, and the two of them left the control area for the computer equipment room, where they were acoustically separated from the rest of the facility.
The anesthesiologist was reported to have been yelling to inquire about the status of the oxygen supply, alarmed by the deteriorating condition of the patient in the MRI scanner. Coincidentally, a nurse, who had come to the MRI suite accompanying a prior patient earlier that day, admitted herself into the working area of the MRI suite to retrieve an item which she had left earlier. Upon hearing the anesthesiologist’s calls for oxygen, the nurse noticed portable cylinders in a patient preparation alcove, directly across from the entrance to the MRI scanner room. She picked up one of the cylinders and handed it to the anesthesiologist who turned to take it to the boy in the scanner.
The “always on” magnetic field of the MRI scanner pulled the oxygen cylinder from the grasp of the anesthesiologist, and it flew into the center bore of the MRI machine, where it struck the boy, who died two days later from the injuries.
At least two other projectile incidents were revealed during the litigation as having happened at the MRI facility in the months prior to the Colombini fatality. One alarmingly similar incident involved an anesthesiologist who brought several ferrous oxygen cylinders into the MRI scanner room. The other involved technologist #1, who was to have administered Michael Colombini’s MRI scan, who brought a ferromagnetic wheelchair into the MRI scanner room. Neither incident was reported to the hospital administration, nor to state or federal officials.
With these facts—which portray not only the events of the single day of the accident, but also something of the organizational and safety culture at UIMA and WMC—it is possible to trace the outcomes of this accident to more than 50 contributory root causes.
Root Cause Analysis
| |
|
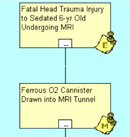
| Figure 1: Colombini Logic Tree Event and Mode |
 With these facts, we can drill-down in a root-cause analysis (RCA) to a set of practical lessons based on the construction of a “logic tree.” A logic tree is a graphical representation of cause-and-effect relationships that led to an undesirable outcome. Essentially it starts with the facts known about the case and works backwards in time to unfold the path of failure leading to the incident.
With these facts, we can drill-down in a root-cause analysis (RCA) to a set of practical lessons based on the construction of a “logic tree.” A logic tree is a graphical representation of cause-and-effect relationships that led to an undesirable outcome. Essentially it starts with the facts known about the case and works backwards in time to unfold the path of failure leading to the incident.
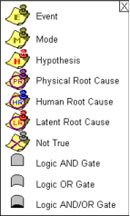
Our logic tree starts with an Event (E). The Event is the last effect in a chain of cause-and-effect relationships. The Event is a fact. At this point we ask “How did the event occur?” The answer is labeled M for ‘Mode.’ (Figure 1).
At this point in an investigation, these are the facts that are known. It is here where we start to hypothesize and ask, “How could the events in the previous block have occurred?” We seek to move backwards, in short increments of time, to unfold the sequence of events and to use collected evidence to support or refute the hypotheses.
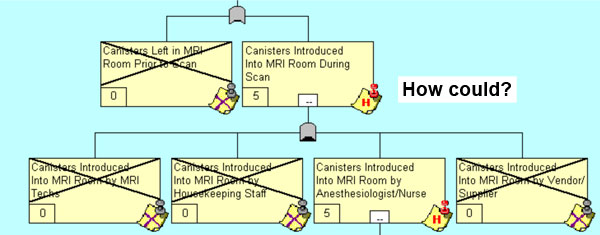
By asking, “How could the ferrous O2 canister have been drawn into the MRI tunnel?” we hypothesize that either the canisters were left in the MRI room prior to the scan or the canisters were introduced into the MRI room during the scan (Figure 2).
 |
|
| Figure 2: ‘How Could’ Questioning Process |
Now that we have hypotheses, we need to validate which are true and which are not. The numbers in the lower left hand corner of each block is a Confidence Factor. This is the degree of confidence we have in the supporting evidence. The scale is from 0 to 5 where 5 indicates conclusive confidence and the hypothesis is therefore true. This degree of confidence will come from the Verification Log. In Figure 3 we can see a sample of the verification log for the hypothesis about the canisters being introduced into the MRI room during the scan. This is essentially our evidence log that captures the verification method used, the outcome, any file links to support the hypothesis, the person responsible for collecting the data, and the date by which the verification data would be collected.
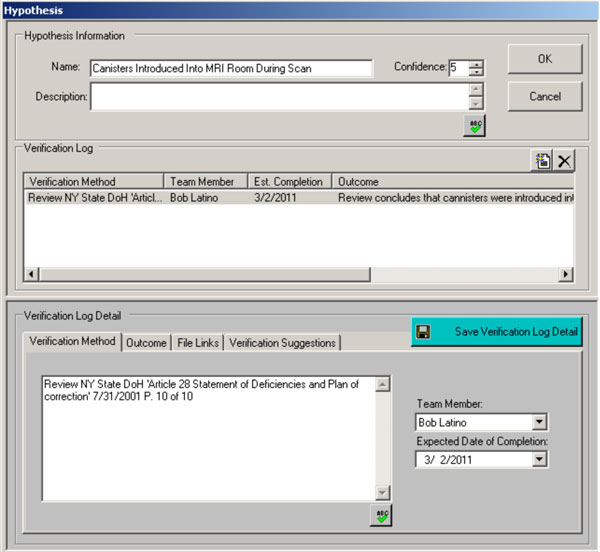
Figure 3: Sample Verification Log
So the questioning and validation process continues as we progress backwards in time and re-create the path of failure. In Figure 4, we show the next level of questioning and the resulting six paths of simultaneous contribution to the overall incident.
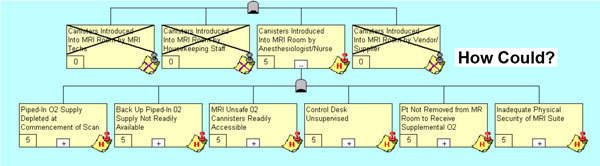
Figure 4: The Next Level of ‘How Could’ Questioning
As this questioning process continues, we drill past the symptoms and deeper into the systemic issues that really triggered poor decision-making. By following the “Piped-In O2 Supply Depleted at Commencement of Scan” box we can conclude the string of logic depicted in Figure 5.
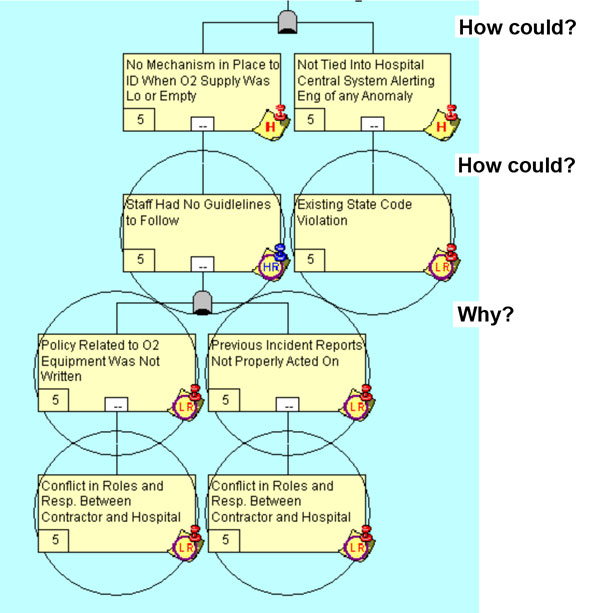
Figure 5: The Uncovering of Latent Root Causes
When we get to a point on our logic tree where a decision has been made (Human Root [HR]), we now switch our questioning to “Why’?” At this point we seek to understand the rationale for a specific decision and asking “Why?” is more appropriate.
In this single string of logic, based on the evidence collected, we see 1) a conflict in roles and responsibilities between the contractor and the hospital and 2) violation of existing state codes.
The conflict in the roles and responsibilities is illuminated in the deposition transcripts, which show that the MRI technologists were unclear on both the immediate responsibility for checking the MRI’s bulk oxygen cylinder and the larger issues of whether maintenance and upkeep of the MRI oxygen supply was the responsibility of the hospital or the MRI center. While safety is not inherently compromised when an imaging facility is operated by a third-party contractor, the structural separation between hospital and MRI operations required a level of communication and coordination that was clearly absent in this situation.
Further evidence of this communication gulf was demonstrated when two prior MRI projectile accidents (neither resulted in injury) were discovered to have happened at the same facility in the months and years prior to the Colombini accident. The concealment of these accidents from the State of New York violated the Department of Health statutes, and the failure to communicate prior accidents within the institution (including a prior accident that involved ferromagnetic oxygen tanks, and the remediation step, which included using only non-ferromagnetic oxygen tanks within the MRI suite) contributed to the Colombini accident.
Of course this is only one leg of the logic tree but it shows how systemic causes (Latent Roots [LR]) influence our decision-making processes.
From these causes, a provider could identify a specific set of operational protections. For the failure of the piped-in oxygen system, these operational protections might include:
- MRI staff training on the operation of the medical gas system, including zone valves.
- Established responses for pressure/flow failures of medical gas service, including support from engineering.
- Exercised code procedures, which might include the use of MR-conditional portable medical gas cylinders and/or MRI scanner room evacuation.
Following this process for the rest of the logic tree resulted in the summary of root causes outlined previously. For a narrated tour of the complete logic tree, please visit www.reliability.com/mri/.
A Reflection on MRI Safety 10 Years Later
The American College of Radiology’s MR Safe Practice Guidance Document was initially published in 2002 following an investigation of the Colombini fatality by the committee’s appointed chair, Dr. Emanuel Kanal. Corrective measures to nearly all of the contributory causes are contained in the ACR’s publication, the contemporary version of which is titled ACR Guidance Document for Safe MR Practices: 2007 (see below).
While the ACR Guidance Document (and its predecessor versions) does contain comprehensive and effective protective measures, no organization—including the ACR, which sponsored the development of the tool—requires its safety provisions for facility or MRI-specific accreditation (this despite the explicit request of the ACR’s own MRI safety committee in 2006). Though the ACR publicly announced in 2009 that they would be integrating Guidance Document provisions in their MRI accreditation requirements, in 2010 they indefinitely postponed that effort, citing bureaucratic burden as a result of the College’s new participation in the CMS outpatient imaging accreditation requirement.
The Joint Commission (TJC) has published articles for its members and, most importantly, a Sentinel Event Alert, the Commission’s highest patient safety warning, about MRI accidents and injuries. Inexplicably, however, TJC did not select any of the performance criteria from Sentinel Event Alert (SEA) Issue #38: Preventing Accidents and Injuries in the MRI Suite for on-site survey review in the years following its release, though it did so for elements in other SEAs. Furthermore, TJC has disavowed that its own SEAs should be required elements of an accredited hospital’s Environment of Care risk assessment (providing a risk assessment of the services and environment is a requirement of Joint Commission accreditation).
In a positive development, Michael Kulczycki, executive director of The Joint Commission’s Ambulatory Care Accreditation Program, has stated that the organization will soon be providing extensive MRI safety training to its hospital surveyor corps, a first for the organization. While it is unclear what the expectation will be for TJC accredited providers, we expect increased attention to MRI safety concerns to be part of upcoming surveys.
Given the lack of response from regulatory, licensure, and accreditation bodies to the known risks (and published protections) for MRI, one might conclude that individual providers have been left to determine for themselves what MRI safety efforts are appropriate because the current system has been proven effective at managing MRI adverse events. That would make sense if the time frame from 2004 to 2009 did not record a 472% growth in the incidence of FDA-reported MRI adverse events.
In a period of five years, we witnessed growth of nearly five-fold in the number of MRI accidents. Among these events were impalements, severe burns, crushing injuries, medical device interactions, and deaths.
So, 10 years later, it appears that the knowledge of the risks and causes of MRI accidents has been captive in institutional ivory towers. In the 10 years following this infamous accident, the professional accreditation bodies with the greatest capacity to mitigate these incidents have not taken a stand that would compel their members to implement these protections. The persistent down-stream effect has been (and continues to be) that avoidable serious injuries to patients and caregivers not only continue but are growing at an alarming rate.
The RCA of this one accident does not provide us a window into the full range of contemporary MRI risks, or even all MRI hazards of 2001. It does, however, plainly illustrate that elements foundational to effective safety programs beyond MRI (training, appropriate facility design, comprehensive and up-to-date policies and procedures, clear lines of communication and authority) are equally relevant to MRI.
Beyond these common foundational elements, there are safety needs unique to MRI, such as access restrictions, non-magnetic equipment, ferromagnetic screening, specific hazard warning signage, all of which would help to prevent a recurrence of just this sort of accident.
The value in this RCA lies in exposing the “Russian doll” nature of this one accident, revealing both the immediate decisions and the persistent, underlying latent causes that led to the tragic outcome. There are more than 50 boxes of individual inquiry in the Colombini RCA, which we can’t fully explore in this article. The reader is invited to view the full product of the analysis, available online at www.reliability.com/mri/.
Toby Gilk is an MRI safety expert and is both president and MRI safety director for Mednovus Inc. (www.Mednovus.com) and senior vice president for RADIOLOGY-Planning (www.RAD-Planning.com). He also is a former member of the American College of Radiology’s MRI Safety Committee. Gilk may be contacted at Tobias.Gilk@Mednovus.com or TGilk@RAD-Planning.com.
Bob Latino is an internationally recognized expert in the field of root cause analysis (RCA) and CEO of Reliability Center, Inc. (www.reliability.com), a consulting firm specializing in improving equipment, process and human reliability. Latino may be contacted at blatino@reliability.com.
References
The ACR Guidance Document for Safe MR Practices was published after the Colombini accident, and it clearly responds to many of the contributory causes of this accident.
|