Data Trends: Epidemiology and Impact of Patient Falls in Healthcare Facilities
March / April 2009
![]()
Data Trends
Epidemiology and Impact of Patient Falls in Healthcare Facilities
In the National Patient Safety Goals (NPSG), The Joint Commission (TJC) has emphasized the need to reduce the risk of patient injuries from falls due to their high prevalence and associated adverse outcomes in at-risk patient populations. The American Nurses Association’s Magnet Recognition program includes falls as one of the core indicators of performance. Hospitals have devoted quality improvement and research efforts to prevent falls, but patient falls nonetheless consistently compose the largest single category of self-reported incidents in acute care facilities (Joint Commission, 2005).
In the evolving environment of pay-for-performance (P4P), hospitals have a financial stake in reducing the number of fall-related injuries that occur within the environment of care. CMS incorporated falls as a category under the Hospital Acquired Condition (HAC) regulations that became effective October 1, 2008, where hospitals will not receive payment for treating injuries caused by falls that occur in hospitals. An estimate of the average DRG payment for injuries sustained by a patient falling from bed is $24,962 (IPPS, FY 2009).
To institute evidence-based interventions, healthcare organizations first need to study and better understand the characteristics of falls and their prevalence within their facilities. Fall data is usually captured through incident reporting programs. Self-reporting programs with structured data are usually best as they provide valuable insight for facilities when addressing interventions.
For this study, characteristics associated with inpatient falls have been identified using a large cross-sectional sample of blinded data from self-reported incidents aggregated within QComparative™, a de-identified national comparative repository. Data for this analysis came from facilities using the same electronic event reporting system (eERS) — Quantros SRM™. Using Quantros SRM, facilities collect data on actual falls and fall near misses, along with a number of data elements about the event, such as age, location, timing, conditions, and impact associated with a fall. In 2007 and 2008, QComparative contained 50,455 actual reported falls from all types of healthcare facilities. The number of falls reported represented about 13% of all self-reported events within the 2-year period, and has remained consistent quarter over quarter.
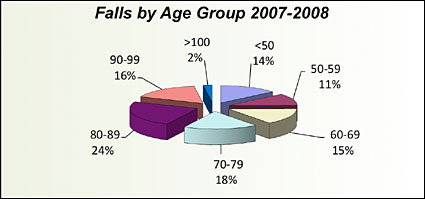
Age has frequently been associated with falls; the data is consistent in QComparative, where the greatest percentage of falls (58%) is in the 70-to-99-year age groups (Figure 1), with slightly more females than males having experienced a fall. Facilities can use age upon admission as a reliable screen for probability, or risk, of fall for a patient, and place such patients in a pathway for higher preventive care or increased frequency of monitoring.
![]()
|
|||||||||||
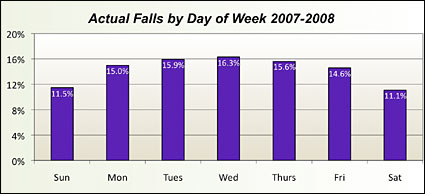
Reported fall rates did not vary appreciably by day of the week or by the time of the day (Figure 2). Weekend days seem to have fewer falls than Wednesday, the highest day. This fact needs further exploration to identify any cause for the variation and to determine its significance to care delivery. Time of day was analyzed by three 8-hour shifts, and we found a slightly increased rate in the 7 a.m. to 3 p.m. shift (Figure 3).
![]()
![]()
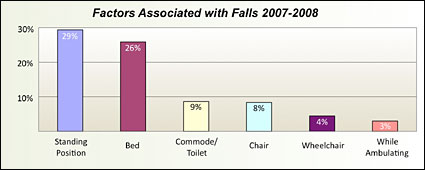
Seventy-four percent of the falls were not observed, and 29% were from a standing position (Figure 3). The epidemiology of hospital inpatient falls in the United States reported by Hitcho and Associates (2004) showed that 19.1% occurred during ambulation, 10.9% when getting out of bed, 9.3% while sitting down or standing up, and 4.4% while using the bedside commode or toilet. Data from the QComparative repository of falls shows a somewhat different pattern.
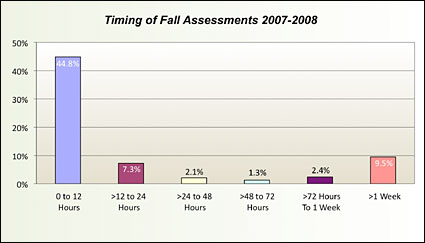
Falls have been identified as a nursing sensitive indicator. Such measures “have a strong ideological connection to quality nursing care” (Moore, 1999) and are used to monitor performance within units and at the facility level. The assessment of the risk of falling is a key component of any fall prevention program (Tzeng, 2008). Results from our analysis reveal that 59% of patients who fell had received a fall assessment. Forty-five percent received this assessment no more than 12 hours prior to the reported fall (Figure 4). This clearly indicates that conducting a fall assessment does not necessarily lead to a reduction in falls. It is most important to actively manage patients to prevent falls from occurring, especially in identified at-risk patients, using higher levels of care management and monitoring is critical. Assessing risk without acting to mitigate falls only adds to the increasing cost of caring for patients.
![]()
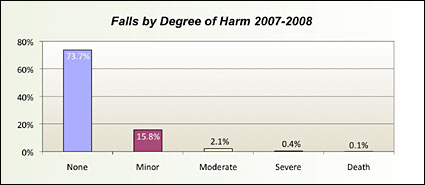
Categorizing falls and the associated degree of harm is helpful in understanding the magnitude of the events. Events ranged from those that produced no harm to those that resulted in the patient’s death (Figure 5). Falls were correlated to the degree of harm as shown below, with the majority of patients experiencing the incident with no harm identified. Even falls that result in minor to moderate harm may add significantly to the cost for the episode of care for that stay. Patients who fall may require extended stays, more tests, additional procedures, and extra monitoring.
![]()
In conclusion, with the risk of harm, increased length of stay, higher cost, and the potential for non-reimbursable costs, falls continue to be an important area on which all healthcare providers need to focus. Using electronic event reporting systems to collect, analyze, and manage events supports providers’ access to key information needed in order to measurably demonstrate reductions in related mortality, morbidity, and cost of associated care.
References
American Nurse Association Magnet Recognition program. Available at: http://www.nursecredentialing.org/Documents/Magnet/MagnetManualKeyChanges.aspx. Data Collection Requirements, pg. 2, and Target for Benchmarked Outcomes, pg. 3.
Inpatient Prospective Payment System (IPPS), Fiscal Year 2009. Final Rule Available at: http://www.cms.hhs.gov/HospitalAcqCond/06_Hospital-Acquired_Conditions.asp
Joint Commission. (2005). Defining the problem of falls. In I.J. Smith (Ed.), Reducing the risk of falls in your health care organization (pp. 13-27). Oakbrook Terrace, IL: The Joint Com mission on Accreditation of Health care Organizations, as cited in Tzeng (2008)
Joint Commission. NPSG 9 – Patient Falls, Available at: http://www.jointcommission.org/AccreditationPrograms/Hospitals/Standards/09_FAQs/NPSG/Patient_falls/NPSG.09.02.01/Fall+reduction+program.htm
Moore, et. al. (1999). Implementation of the ANA Report Card. Journal of Nursing Administration, 29(6), 48-54. Cited in http://nursingworld.org/mods/archive/mod72/ceomfull.htm
National Quality Forum. Nursing care quality at NQF. Available at http://www.qualityforum.org/nursing/#measures
Tzeng, et. al. (2008). Nurses’ solutions to prevent inpatient falls in hospital patient rooms. Nursing Economics, 26(3), 179-187.
