 |
 |
 |

September / October 2008

Cardiac Telemetry Guidelines Improve Bed Utilization and Resources
By Aman D. Sabharwal, MD; Mitchell G. Mason, RN, BSEd; Richard Lapin, MD
Jackson Memorial Hospital is a 1,600-bed tertiary care facility in Miami, Florida, and serves as the primary teaching hospital for the University of Miami — Miller School of Medicine. At one time, the majority of the medical services were teaching services run by house staff physicians; today approximately half of the general medical inpatient services are run by the non-teaching hospitalist services.
Much like other institutions, Jackson Memorial Hospital was experiencing an increased need for adult cardiac telemetry beds, to the point where an excessive number admitted patients were waiting in the emergency services department for telemetry beds daily. While some suspected that many of the patients did not truly require telemetry, we needed to perform a study to validate or refute the suspicions.
A Telemetry Utilization Review project was implemented by the directors of inpatient services in conjunction with the Patient Placement Center. This project was implemented for several purposes:
- to evaluate whether patients currently on telemetry still required continuous cardiac monitoring,

- to evaluate the length of time patients remained on telemetry,

- to improve the emergency department's throughput, and

- to evaluate the potential need for additional telemetry beds within the adult medical division.
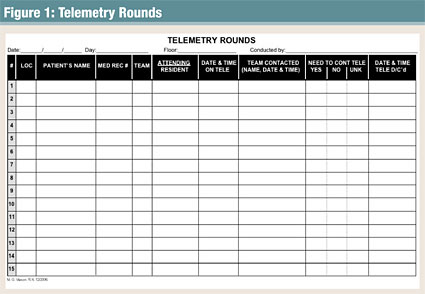
An audit tool (Figure 1) was developed and implemented to determine if patients currently admitted to telemetry truly needed to continue with cardiac monitoring or if telemetry could be discontinued. The associate medical director of inpatient services, who reviewed each chart and discussed the patients' needs with their admitting physicians or teams, completed the utilization review twice a week. The clinical decision of need was based on the guidelines set forth by the American College of Cardiology (ACC; Emergency Cardiac Care Members, 1991). On the first day of the audit, more than 50% of the patients on telemetry monitoring were identified as not requiring further monitoring and were subsequently discontinued after case-by-case discussions were held with the admitting physicians. Over the course of 6 months, over-utilization of telemetry was prevalent during each audit. A total of 736 charts were reviewed from the two telemetry wards, of which 651 were ordered for and were placed on telemetry. Of the 651 telemetry patients reviewed, 354 (54.4%) were identified as no longer meeting the criteria set forth by the ACC. The audits also revealed 120 (18.4%) of these patients did not meet any criteria for cardiac monitoring upon admission (Table 1, pg. 28).

|
 |
 |
 |

















|
 |

