 |
 |
 |

November / December 2007

Collaborative Model Leads to Improved Patient Flow
How a large health care system used a collaborative model to share knowledge and spread information.
By Dennis O'Hare, MD

Laura McElroy, MHA, MBA
The wave of hospital consolidations in the 1990s introduced many healthcare leaders to the complex issues that challenge the management of larger systems (Luke et al.,1995). One such challenge is the spread of information. Knowledge transfer can be difficult in large organizations such as hospital systems where divisions lack a shared social identity or culture (Kane et al. 2005). Upping the ante on the challenge was another evolution in healthcare: the trend toward increased collaboration (Ashcroft, 1996). As defined by Himmelman (1996), collaboration involves going beyond exchanging information to altering activities and sharing resources in the service of enhancing the capacity of another for a common purpose.
At Allina Hospitals & Clinics, newly aligned hospitals were charged with the task of collaborating on a system-wide initiative to improve patient flow. Allina, like hospitals across the U.S. (Haraden & Resar, 2004), struggled with patients waiting to be discharged or admitted, emergency department (ED) patients sometimes leaving without being seen, and ambulances sometimes diverted to other facilities.
National research shows these disruptions in patient flow can place patients at risk, prolong patients' pain and suffering, and affect patient satisfaction and staff satisfaction (Derlet & Richards, 2000). There is a paucity of research available detailing specifics on how, exactly, patient flow issues affect quality of care (Haraden & Resar, 2004). However, some studies have examined how patient flow issues can affect hospital resources. a study of ED patients with chest pain, for example, concluded that hospital revenues were reduced by over $200 for each patient waiting more than 3 hours for a hospital bed (Bayley et al., 2005). a study using a community hospital's historical data showed ambulance diverts and left-without-being-seen (LWBS) patients may have resulted in a loss of more than 3.8 million dollars in revenue in a 1-year period (Falvo et al., 2007).
Complicating the issue is widespread skepticism about healthcare professionals' ability to influence patient flow. Traditionally, providers have collectively thrown up their hands in the face of surges in demand, assuming that the timing of patients' illnesses cannot be predicted. However, research has suggested that daily surges from elective care far outweigh daily surges from emergent care (Haraden & Resar, 2004).
Allina: a System in Progress
Allina Hospitals & Clinics of Minnesota is a nonprofit healthcare system including 11 hospitals and 42 clinics with a combined total of 1,677 staffed hospital beds, 220,000 emergency care visits, and 103,000 inpatient hospital admissions per year. In 2003 a new CEO and leadership team was appointed and a new system-wide strategic plan was developed with the goal of greater alignment and integration of the diverse group of hospitals and clinics. One major goal of the strategic plan was electronic medical record (EMR) implementation, which consumed attention and resources for the next 3 years. In the midst of the new strategic plan and EMR implementation, leaders decided also to focus on patient flow.
In the fall of 2004, Allina joined the IHI Learning and Innovation Community devoted to patient flow (IHIa). a Learning and Innovation Community is defined by IHI as a "collaborative change laboratory" where teams from a wide variety of healthcare organizations rapidly test and implement change within a specific topic area (IHIb). At the same time, Allina's senior leaders were considering how to develop a learning and knowledge network to spread best practices throughout the Allina system. The IHI Learning and Innovation Community on patient flow provided an opportunity to test such a model for information spread and collaboration.
Measuring and Defining Improved Patient Flow
The success of the internal collaborative model would be evaluated through learning session participant surveys and agreed-upon improvement indicators. The system-wide outcome metrics for the patient flow initiative were:
- Adjusted bed turns. In the IHI Learning and Innovation Community, adjusted bed turns were defined as the number of times a functional bed turns over during a specified time period, adjusted by case mix index and average length-of-stay. After reviewing recommendations provided by the IHI hospital flow diagnostic tool (IHIc) and internal data on current bed turns, Allina decided on a target system goal of 100; e.g. the goal was that each bed would theoretically turn over an average of 100 times per year, with adjustments in the number to account for case mix and average length-of-stay. Baseline metrics showed Allina's system-wide 2005 rate to be 103.66 average bed turns per year; some Allina hospitals were under 100 but most were over 100.

- Direct-admission diversions and transfers to another facility. In effect, this measure was rural and suburban hospitals' version of ED diversions; these hospitals, because they are located farther apart, often must admit and treat patients before transfer to ensure patients are stable. Allina's rural and suburban hospitals determined that in 2005 there was a system-wide average of 17.83 episodes per month. (Because some individual hospitals did not gather data for all 12 months of 2005, some of these data were extrapolated.)

- ED diversions. This was defined as the system-wide monthly average of episodes where urban and suburban hospital EDs were closed to ambulances. a 2005 baseline rate was calculated to be 10.36 average episodes per month.

- Left without Being Seen (LWBS) patients. This was defined as the number of checked-in ED patients who leave before being treated or seen by a physician divided by the total number of ED visits. Data aggregated from Allina hospitals showed an average of 2.33% patients were LWBS patients in 2005 with a higher percentage in urban hospitals and a lower percentage in rural and suburban hospitals.
Launching the Internal Collaborative
In the summer of 2004, the Optimal Access Steering Council (OASC) was formed to oversee the patient flow initiative and develop the internal collaborative model that would be used for future system-wide initiatives. The OASC was comprised of senior leaders who represented Twin Cities area hospitals, regional hospitals, and Allina's ambulatory sites. The OASC also included a representative from the system's electronic medical record implementation initiative and a project manager. The OASC was chaired by a senior-level physician champion. Its sponsor was the executive vice-president of quality, safety, and technology.
Work began with a series of regular meetings to clarify metrics and to identify roles and responsibilities during the internal collaborative. The goal was to develop metrics that would provide a system-wide picture of progress, and also be useful for monitoring teams' localized improvements over time. The OASC finalized a document that detailed the scope of the internal collaborative work to be performed and a reporting structure. Managers' incentive plans were linked to results in the system-wide patient flow outcomes. Monthly reports would be shared with the OASC and with the hospital presidents to whom OASC members reported. Hospital teams in the collaborative were charged with the responsibility of deciding on the best strategies for improvement in their unique environments.
In the fall of 2004, Allina joined the IHI Innovation Community, Improving Patient Flow through Acute Care Settings. As part of its plan to use an internal collaborative model built around the "train the trainer" concept, the OASC developed a request-for-proposal to determine which of Allina's 11 hospitals would be chosen to attend the IHI Innovation Community and also take on the role of trainers. Applicants answered questions about how their team would utilize the information gleaned and share what they learned with the other hospital teams in the Allina system. First one, then a second team was chosen to actively participate in the IHI events.
In February 2005, Allina launched the Allina Patient Flow Internal Collaborative. Each hospital was required to appoint one multidisciplinary team to the collaborative, which typically was comprised of representatives from the emergency department, a case manager, a physician champion, RNs from selected nursing units, as well as other stakeholders.
In the beginning, the collaborative served as a forum for team input that would refine and finalize metrics. In 2005, meetings were used to allow teams time to plan implementation strategies at their individual hospitals. Because of this, the OASC decided that 2005 would be the baseline year for patient flow metrics; implementation of the initiative would occur in 2006 and 2007. (See Table 1.)
Summer 2004 |
Allina forms OASC to create internal collaborative model and oversee patient flow initiative. |
Fall 2004 |
First of two Allina teams joins IHI Innovation Community. |
February 2005 |
Allina internal collaborative launched. |
February 2005
December 2005 |
A second Allina team joins the IHI Innovation Community. The teams report on what they've learned through IHI. Other time during internal collaborative meetings is used to:
- Discuss and refine metrics

- Plan for hospital-specific implementation

- Collect baseline data.
|
January 2006 |
Patient flow initiative officially launches. Initiative is declared to be a two-year initiative. |
January 2007 |
First full year of data are analyzed and show improvements. |
|
|
Through discussions at OASC and refinement at collaborative meetings, final metrics were established. Four types of metrics were used. Process measures helped identify whether staff members were producing the work necessary to reach goals. Intermediate metrics captured a hospital's individualized progress toward system-wide outcomes and provided a more immediate goal to which teams could aspire. Balance metrics helped identify whether changes within the hospital were having untoward effects. For example, readmission rates were monitored for changes that might be related to more efficient discharge times. System-wide outcome metrics were the overall system goals that system leaders wanted to reach. System-wide outcome metrics were the only metrics that were not determined by individual hospital teams.
The process for ensuring for internal knowledge transfer and collaboration among collaborative team members consisted of three elements:
- Twice-yearly learning sessions. All teams, collectively about 100 employees, attended these events, which featured a prominent national expert on patient flow who was retained to discuss concepts and topics requested by teams. Each hospital team was required to create a storyboard to share with other teams. Teams reported that the storyboards provided an opportunity for them to focus on their own accomplishments, as well as an opportunity for recognition from their peers. The system CEO and other system executives, including the executive vice president of quality, safety, and technology, made opening remarks at the sessions and hospital presidents were invited for the portion of the day when their hospital's team reported.

- Video-conferenced, monthly workgroup meetings to share tools and review progress. There, team leaders who attended the IHI collaborative discussed what they learned through their involvement in the program. All team leaders then participated in a structured dialogue where relevant experiences were shared and teams disseminated effective tools and measurement tactics. Finally, individual teams determined their next steps by answering the following questions: What outcome metric are we trying to move? What intermediate metrics will help? What can we do this month to improve that metric? What will we do next month?

- An internal knowledge-management structure. Regular updates were provided to all team members, selected senior leaders, and any Allina staff member who requested it via an email newsletter called Go with the Flow. This electronic resource provided recent articles and tools and highlighted teams for their successes. The newsletter linked to an Intranet site where employees could review additional articles, submit their monthly data, and see a schedule of upcoming events.
Results
Surveys completed after in-person internal collaborative learning sessions showed that participants perceived the sessions to be valuable sources of information. At the lowest-scoring learning session, 91% of participants agreed or strongly agreed that the session provided useful tools and knowledge and 91% of participants agreed or strongly agreed that they would be able to apply what they had learned. At the highest-scoring learning session, 96% of participants agreed or strongly agreed that the session provided useful tools and knowledge; 96% of participants agreed or strongly agreed that they would be able to apply what they had learned.
In addition, at the conclusion of the first year of the 2-year patient flow initiative, several system-wide measures showed improvement (Table 2). By the end of 2006, hospitals achieved a system-wide decrease in left without being seen (LWBS) patients. In 2005, an average of 2.33% patients were LWBS patients. In 2006, an average of 2.17% were LWBS patients.
Measure |
Definition |
2005 Baseline |
2006 Results |
Bed Turns (Adjusted) |
((# admissions / # functional/staffed beds) * CMI) + (# Outpts in IP beds / # functional staffed beds) |
103.66 |
108.22 |
ED LWBS Rate |
# of ED patients that check in at the triage desk in the emergency dept but leave before being seen by a physician or being treated* / total number of ED visits |
2.33% |
2.16% |
Number of ED Diversions (METROS) |
Number of times the ED "closed" to ambulances |
10.36 |
8.92 |
Number of Direct Admit Diverts and Transfers to another facility (REGIONALS) |
Number of times the hospital was closed to "direct admits" and number of times a patient was treated then transferred to another acute care facility due to capacity issues |
17.83 |
18.83 |
|
|
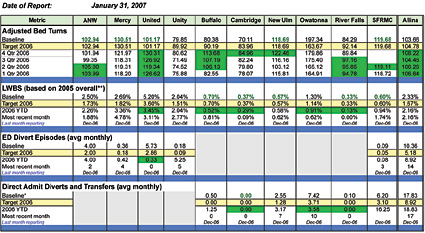
Baseline metrics for 2005 adjusted bed turns showed a system-wide rate of 103.66 average bed turns. Because the number exceeded the goal of 100 average bed turns in Allina hospitals, hospitals with individual rates over 100 bed turns sought to maintain their rate while hospitals below 100 worked to improve. In 2006, the system-wide average rate of bed turns increased to 108.22.
Allina also made progress on emergency room diverts by the end of 2006. The 2005 average number of diverts per month was 10.36. The 2006 average number of diverts per month was 8.92.
Several teams realized notable goals in individual progress. An example is Allina's 400-bed United Hospital, which met all of its 2006 patient flow metric goals. For example, in 2005, United had an average of 5.73 ambulance diverts per month. In 2006, they had an average of 1.5 ambulance diverts per month and had gone 5 months in 2005 with zero diverts. United also reached its goal of reducing LWBS patients from its 2005 baseline rate of 5.2% to 3.59%.
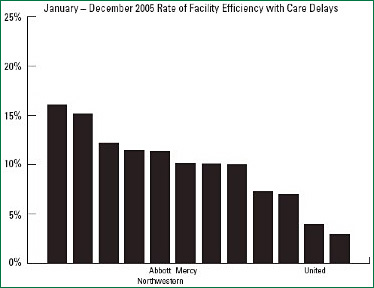
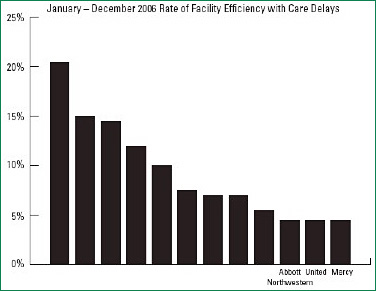
Allina's improvements in patient flow efficiencies also were noticeable in a community-wide comparison of health facilities' care efficiency. The community-wide comparison is regularly undertaken by the health plan division of HealthPartners, an integrated health care system in Minnesota, which uses the data to evaluate their provider network. Part of the comparison involved monitoring of percentages of admissions that experienced delays affecting patient flow. (Examples included delays in performing diagnostic testing, delays in execution of orders, and delays in social service interventions.) In 2005 at the beginning of the patient flow collaborative, the three Allina hospitals who participated in the comparison United, Mercy, and Abbott Northwestern were 2nd, 7th, and 8th respectively out of 12 Twin-Cities-area facilities being compared for efficiency. The percentage of admissions that experienced delays in these facilities was 5% for United, 11% for Mercy, and 12% for Abbott Northwestern (Figure 1). In 2006 at the end of the first year of the patient flow collaborative work, the three Allina facilities had become the best performers in the network for this set of measures. The percentage of admissions that experienced delays was at 6% for all three hospitals (Figure 2).


It should also be noted that Allina was simultaneously implementing their electronic medical record (EMR). Several hospitals were actively going live during this time frame, which negatively affected their individual, and our composite, flow efficiency and results.
Discussion
When the patient flow initiative was undertaken, Allina system leaders were building their experience with implementing a major initiative as a large, multi-location organization. Significant time was required to reach agreement on roles, responsibilities, and definitions of system-wide metrics. It was helpful that some measures were left to individual hospitals, such as hospital-specific intermediate metrics, process measures, and balance measures to ensure that patient flow changes weren't adversely affecting other parts of a hospital. Several of the tactics utilized to help ensure success are captured below:
Rapid-cycle improvement testing. The freedom to choose strategies for improvement empowered teams to make frequent use of Plan-Do-Study-Act (PDSA) cycles (Deming, 2000). PDSA cycles have been used extensively in healthcare and other industries to test changes on a small scale and understand how those changes affect other departments. Since the flow of patients touched every department in a hospital, small changes to patient flow sometimes had far-reaching, unintended effects. The PDSA cycles allowed teams to understand the real effect of a change before committing to the change in a large-scale way. Reports of PDSA tests at the monthly workgroup meetings allowed successful practices to spread quickly to similar hospital environments.
Progress visuals. a metric dashboard tracked indicators for key system-wide goals. The use of an effective dashboard was instrumental in keeping an organizational focus; the dashboard was distributed to key stakeholders and results were reported and reviewed monthly during OASC meetings (See Table 3). Metrics from the dashboard were included on an overall Allina dashboard for key goals in Allina's overall operating plan. The access initiative was represented in overall Allina dashboard through two of the measures: LWBS and ED diverts.

Senior-level accountability. Senior level accountability helped teams in the collaborative maintain focus. Manager incentive plans prompted OASC leaders to support and drive team improvements while leaving methods of improvement to individual teams. Visits to learning sessions by the CEO and executive vice-president of quality, safety, and technology were helpful in demonstrating to teams the importance of their work.
Dedicated project management expertise. The internal collaborative model greatly benefited from centralized, ear-marked resources in the form of a dedicated project manager/consultant as well as dedicated time from Allina's measurement and analysis department. This support illustrated leaders' commitment to the program by allocating the needed resources to ensure its effective management. The project manager, who had an extensive process-improvement background, was hired specifically for the patient flow initiative and was utilized by individual teams across the system to help with appropriate goal-setting. Her credibility as a professional with a deep understanding of process improvement helped to guide the collaborative teams toward success.
Work coordination. OASC members' links with other key system initiatives were critical to success. At Allina, electronic medical record implementation was a major focus at the same time the patient flow steering committee was launching. a representative from the EMR team sat in on OASC and internal collaborative meetings and brought back information that helped EMR software developers design a system that would serve patient flow needs. For example, prior to the EMR, many hospitals used charting which included slots for anticipated and actual discharge times. Initially, EMR software deleted the anticipated discharge time in the chart as soon as an actual discharge time was entered. This would have prevented teams from determining whether discharge time goals were being met. While leaders had expected that implementing two major initiatives at the same time may temporarily slow down improvements in both areas, both patient flow and EMR implementation were successful. In fact, in 2007, Allina won the HIMSS Nicholas E. Davies Award of Excellence for its success in EMR implementation.
External expertise. Participation in the IHI Innovation Community was invaluable to Allina's success. The internationally recognized thought leader provided through IHI helped drive creative exploration and encouraged Allina teams' commitment during the initiative. The work of pioneering hospitals around the country inspired Allina's IHI teams who, in turn, passed on their knowledge and enthusiasm to the Allina teams who were not attending IHI events in person.
Summary
Allina's internal collaborative process has fostered collaboration while facilitating the spread of the latest knowledge throughout a large, diverse organization. Through this application of information sharing and knowledge transfer, Allina was able to achieve improvement in several measures related to patient flow inefficiencies. The organization plans to apply the process to similar initiatives to improve quality in the future.
Dennis O'Hare is the vice-president of medical affairs at Mercy & Unity Hospitals, part of the Allina Hospitals & Clinics system. He may be contacted at Dennis.OHare@allina.com.
Laura McElroy was the project manager for the Allina Hospital Flow Collaborative at Allina Hospitals & Clinics.
References
Ashcroft, B. (1996). Collaboration: More than a buzz word of the '90s. Clin Nurse Specialist, 10(2), 94.
Bayley, M. D., Schwartz, J. S., Shofer, F. S., et al. (2005). The financial burden of emergency department congestion and hospital crowding for chest pain patients awaiting admission. Ann Emerg Med, 45, 110-117.
Deming, W. E. (2000). The new economics for industry, government, education. Cambridge, Mass: MIT Press.
Derlet, R. W., & Richards, J. R. (2000). Overcrowding in the nation's emergency departments: Complex causes and disturbing effects. Ann Emerg Med, 35, 63-68.
Falvo, T., Grove, L., Stachura, R., et al. (2007). The opportunity loss of boarding admitted patients in the emergency department. Acad Emerg Med, 14, 332-337.
Haraden, C., & Resar, R. (2004). Patient flow in hospitals: Understanding and controlling it better. Frontiers Health Serv Manage, 20(4), 3-15.
Himmelman, A. (1996). On the theory and practice of transformational collaboration: Collaboration as a bridge from social service to social justice. In C. Huxham (Ed.), Creating Collaborative Advantage. London: Sage Publishers.
(IHIa). Learning and Innovation Community: Improving Flow Through Acute Care Settings. Available at: http://www.ihi.org/IHI/Programs/InnovationCommunities/
ImpovingFlowThroughAcuteCareSettings.htm
(IHIb). http://www.ihi.org/IHI/Programs/InnovationCommunities/
(IHIc). http://www.ihi.org/IHI/Topics/Flow/PatientFlow/
EmergingContent/HospitalFlowDiagnostic.htm
Kane, A. A., Argote, L., & Levine, J. (2005). Knowledge transfer between groups via personnel rotation: Effects of social identity and knowledge quality. Org Behav Hum Dec Processes, 96, 56-71.
Luke, R., Ozcan, Y., & Olden, P. (1995). Local markets and systems: Hospital consolidations in metropolitan areas. Health Serv Res, 30, 555575.
|
 |
 |
 |


















|
 |



