
May / June 2005

Case Study
Improving Medication Safety with a Wireless, Mobile Barcode System in a Community Hospital
By Mitch Work
Over the past few years, hospital organizations have increasingly looked to new technology solutions to improve patient safety. Barcode technology is an especially promising approach in the effort to reduce medical errors. While barcode technology has been used for quite some time in many hospital applications, it has only recently been used to address patient safety. The use of barcode technology at the patient's bedside has shown impressive gains in reducing medication administration errors, which may account for as many as 7,000 deaths per year in U.S. hospitals (IOM, 2000).
Barcodes provide a valuable verification of medication administration by assuring that the "five rights" are confirmed — right patient, right medication, right dose, right time, and right route of administration. While studies conducted in VA hospitals in the early 1990s showed that the use of barcodes reduced medication administration error rates by up to 86% (Meadows, 2003), community hospitals are just beginning to use this technology to improve patient safety. Recent estimates indicate that only 2% to 6% of hospitals are currently using barcodes to reduce medication administration errors (Center for Business Innovation, 2004).
Background
This case study examines the use of a wireless, mobile barcode medication administration system at Beloit Memorial Hospital in Beloit, Wisconsin, a 175-bed community hospital with four off-site clinics, serving a population of approximately 175,000 residents living in southwestern Wisconsin and northwestern Illinois.
The hospital has a formal affiliation with the University of Wisconsin Hospital System and an active though informal affiliation with Rockford Hospital in Rockford, Illinois. The hospital's Board of Trustees, composed of 10 medical professionals and community leaders, has committed the hospital to a primary goal of providing high-quality healthcare services for all patients.
In September 2003, Beloit Memorial installed a wireless, handheld barcode medication administration system in its Family Care Center (FCC) unit, consisting of 35 ob/gyn, pediatric, and labor/delivery beds. This pilot resulted in a 67% decrease in medication administration errors within the first four months of operation. With the pilot successfully completed, the hospital expanded implementation of the barcode system to four additional inpatient units. This case study documents Beloit's experience in these units, which included:
- Special Care Center (SCC) Oncology

- Multi Care Center (MCC) General Medical Surgical

- Intermediate Care Center (ICC) Telemetry

- Critical Care Center (CCC) Critical Care
These units presented a more complex environment than the FCC, treating patients with generally more serious medical conditions, who often required more medications. Consequently, these units were more prone to experience medication administration errors.
Goals and Objectives
The main goal of this study was to identify and measure the benefits of a wireless barcode system to reduce medication administration errors.
To address this goal the following specific objectives were established:
- Conduct an onsite visit, both pre- and post-implementation of the wireless barcode system in the four new inpatient units.

- Determine pre- and post-implementation medication administration error rates in these units.
Methodology
Pre- and post-implementation site visits were conducted by an independent consultant who interviewed senior nursing management, the unit managers, and the nurses charged with medication administration responsibilities; and observed the medication administration rounds.
The pre-implementation visit was conducted in late June 2004, and the post-implementation visit was conducted in December 2004, to review the results of the system four months after the "go-live" date. This interval was selected to ensure that the nursing staff was familiar with the barcode system and had completed its learning curve of the new system.
Patient Safety Goals
The hospital Board of Trustees and senior management have focused on establishing a culture of cooperation and communication aimed at improving the quality of patient care. This culture was key to embarking on a successful patient safety program. While the hospital established a Patient Safety Committee in 2001, the barcoding initiative originated from a recommendation by the director of pharmacy, who felt that additional checks and safeguards at the point of medication administration would be valuable in reducing medical errors. As a result, the hospital embarked on its initial barcode pilot in September 2003. The alignment of the board and senior hospital management including the CEO, the vice president of nursing, and department heads created a positive atmosphere and communicated a clear, unified message from senior management that led to the adoption and funding of the new barcode system.
Anticipated Benefits
In expanding the use of barcode technology to the additional inpatient units, the hospital hoped to achieve the following benefits:
- Improve patient safety through the reduction of medication administration errors, while minimally increasing nurse staffing time requirements.

- Improve nursing staff job satisfaction.

- Improve patient satisfaction.

- Generate positive public relations with the local community.
Barcode Implementation at Beloit
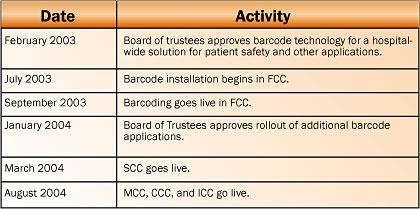
In February 2003, the Board of Trustees unanimously approved funding for a bar-code pilot project in the FCC, which began in July 2003. By January of the following year, the hospital approved the further deployment of barcoding for medication administration to include four additional inpatient units due to the FCC's early success. Implementation of the original pilot and subsequent rollout to the other inpatient units occurred over a 15-month period from July 2003 through October 2004. The SCC went live in March 2004. The MCC, CCC, and ICC all went live in August 2004. This chronology is shown in Figure 1 below.

|

