A Dedicated Urology Triage: Providing Safer, Faster, and More Efficient Emergency Urology Care
By Louise Goldsmith, MBBS, BSc, MRCS
Urology patients have unique primary and secondary care requirements. They are an ever-growing patient population requiring specialist input for their long-term conditions, such as suprapubic catheter changes and nephrostomy flushes. With community services such as district nurses and general practitioners pressured to manage these patients in the community, urology patients often end up being sent into our emergency departments (ED). This fills up the EDs with non-emergency patients and merely transfers the burden of care from one team to another.
Everyone is feeling the strain. Community general practitioners must deal with increasing time pressure on their day-to-day duties and lack the confidence to manage complex urological patients. And hospital urologists are spread thinner, frequently cross-covering multiple sites while on call. Cracks in patient care can appear—with urology patients not always accessing care in the appropriate time frame or from the appropriate team of people.
To combat and resolve this endemic issue, this article describes the evolution, implementation, and outcomes of our dedicated urology triage service.
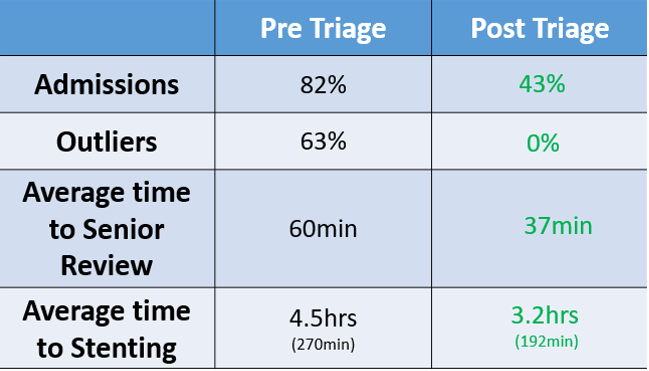
Originally, our urology on-call service cross-covered three sites, with the admitting ED on a different site to the urology department and ward. Acute urology presentations were assessed and admitted via the surgical emergency unit, also on the ED site, resulting in:
- Wasteful fragmentation of on-call resources, as the on-call urology registrar had to travel between the various sites
- 63% of the urology patients outlied at the non-urology hospital site, with morbidity and mortality well-known to increase in patients outlying away from their specialist ward
- Assessment and initial care carried out by junior doctors and nurses without urological specialist skills or on-site senior urology support, causing unnecessary admissions and suboptimal care
All of these factors resulted in delayed urology review and delayed emergency intervention. Interventions for urological emergencies, such as scrotal exploration for a testicular torsion or decompression of an infected obstructed kidney, are time-critical. Therefore, any delay in intervention can only worsen patient outcomes.
Solution
Our answer to this problem was a dedicated urology triage. The triage unit allows admissions onto the same site as the urology ward. Triage is staffed by advanced nurse practitioners with urology-specific skills and by the on-call urology team. Following a business case proposal, funds and a four-bed closed section of a ward were secured to facilitate the unit and allow for assessment and care of acute urology patients. They would be directed straight to the triage unit from ED or the community, once the patient had been discussed with the on-call urology team. This eliminated the need for the on-call registrar to travel between sites, instead directing patients straight to the triage unit. In the current climate of staff and funding cuts, hospitals throughout the UK have empty or closed wards that could similarly serve as urology triage units.
Achievements
Twelve months after the implementation of our dedicated urology triage unit, the admission rate has fallen from 82% to 43%, with problems managed immediately by skilled staff and patients often discharged immediately or later the same day. Time to senior review has dropped from 60 to 37 minutes, which has also reduced time to intervention. Infected obstructed kidneys are now being decompressed on average in 3.2 hours, versus 4.5 hours previously. Time to scrotal exploration has been reduced so that 87.5% of patients underwent scrotal exploration within two hours of the decision to intervene. This resulted in 100% of all torted testicles remaining viable. Patient outlying at the non-urology site was reduced to 0% from 63% previously. Patient satisfaction has also improved, and patient surveys frequently cite efficient care and immediate access to the correct team as benefits.
Reproducibility
Benefits of specialty-specific acute admission units have been demonstrated by surgical emergency units and acute medical units nationwide. Allowing community healthcare practitioners and EDs to directly refer to a specialty admission unit streamlines and improves care for all. The urology triage unit can be reproduced within other urology departments to achieve the same benefits, but it can also be implemented by other medical specialties such as gastroenterology and cardiology. To reproduce this triage model elsewhere, physical space, financial backing, and sufficient volume of urology referrals would be integral to its success and longevity.
Louise Goldsmith is urology registrar at The Churchill Hospital, Oxford University Hospitals, England.
