|
 |
 |

September / October 2008

A Dashboard for the PACU
Given a Window into the OR, Recovery Nurses Transform Work Methods
By Scott Ciesielski, RN, MS; Bethany Daily, MHA; Wilton C. Levine, MD
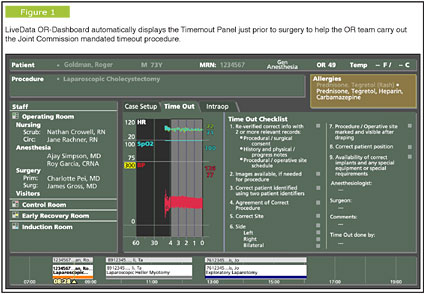
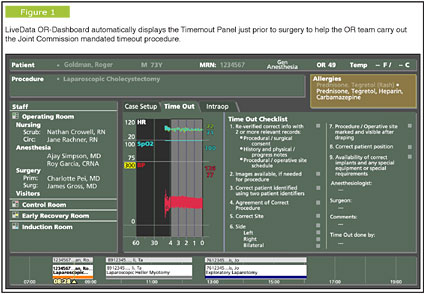
Communication in the perioperative environment is critical for patient safety and effective teamwork. Team members need to know the name of the patient, scheduled procedure, patient precautions and allergies, along with names of team members working together for a given case. Over the past several years, Massachusetts General Hospital (MGH) developed an intra-operative dashboard in collaboration with LiveData (Cambridge, Massachusetts) to aid in the Timeout/Universal Protocol process as well as provide these critical communication elements (Figure 1).

|
 |
 |
 |


















|
 |