 |
 |
 |

November / December 2005

Bed Utilization
New Roles Improve
Bed Utilization
By Aman Sabharwal, MD; Roshan K. Rao, MD;

Janice K. Gonzalez, RN; Mitchell G. Mason, RN, BSEd
Jackson Memorial Hospital (JMH) in Miami, Florida, is an accredited, non-profit, tertiary care hospital and the major teaching facility for the University of Miami's Miller School of Medicine. JMH is one of the busiest centers in the country with approximately 1,500 licensed beds, 225,000 emergency and urgent care visits, and nearly 60,000 admissions to the hospital each year. JMH is the only full-service provider for the uninsured and medically indigent in Miami-Dade County.
JMH has a broad range of tertiary services and clinical programs designed to serve all of this diverse community. Its medical staff is recognized nationally for the quality of its patient care, teaching, and research. The hospital has over 11,000 full-time employees, approximately 1,000 house staff, and has nearly 700 clinical attending physicians from the University of Miami.
Over the last several years a combination of pressures from regulatory agencies and an increasing number of admissions brought the admitting process to a near standstill. Teaching services were (and still are) being held to the admission cap guidelines by the Residency Review Committee (RRC). Ironically, the Accreditation Council of Graduate Medical Education (ACGME) began to enforce strict work hour rules for all training programs. With these restrictions in place, a fixed number of admissions are admitted to a fixed number of services within a shorter period of the day. In fact, many patients were being held in the emergency department (ED) for as long as 15 hours (or more) before an internal medicine service saw the patient or wrote admission orders.
In 2002, JMH nursing executives attended a meeting of the Health Care Advisory Board in Washington, D.C., and identified an urgent need to expedite patient throughput and maximize hospital capacity. Initially the forum's goal was to simply improve ED throughput, however, this led to examining factors that serve as inherent barricades to overall hospital throughput and ultimately impact the hospital's ability to consistently reach maximum bed capacity. Some of these contributing factors included:
- turnaround times for environmental services to clean rooms,

- how long it takes for medications to be dispensed from the pharmacy,

- inefficiencies in registration and admitting processes,

- social workers not being notified early in the discharge planning process,

- poor communications between physicians, nurses, and bed control personnel regarding the appropriate bed setting needed, and

- poor tracking systems, just to name a few.
In the recent past, admitted ED patients at JMH moved to the ED's holding area (ER-H), which serves as a tertiary inpatient setting, or the patients were sent directly to the in-house beds if clean beds were available. If beds were not available, patients waited in ER-H for as long as several days. With the imposed admitting restrictions, an average of 15 patients requiring admission were being held-over each night in the ED for the next day's admitting teams, which impeded the movement of patients throughout the ED.
This posed increased patient safety issues and poor bed utilization within the entire institution. Additionally, ER-H would generally remain empty or underutilized throughout the night as no ED patients were being admitted until the medical teams "re-opened" the following morning. Once the teams re-opened and admission orders were written, a large number of patients would then be transferred to ER-H within a period of a few hours. Furthermore, beds and nursing staff on the inpatient floors were also underutilized until later in the day when the admitted patients were moved from ER-H to available beds throughout the hospital. There were also concerns about patient safety and providing a high quality of care for these patients. We were also concerned that the ED physicians had to care for patients who were essentially inpatients while continuing to treat new ED cases. A survey conducted throughout the institution confirmed these "suspicions."
Patient Placement Coordinators
In an attempt to improve patient care and to maximize bed utilization, the hospital's ED developed two new initiatives. The first of these to evolve was a new position called Patient Placement Coordinators (PPC). The PPC evolved from a group of select senior nurses with strong administrative and clinical backgrounds. Their sole job was to improve ED throughput, improve bed utilization throughout the entire hospital, and to ensure that patients were assigned to in-house settings that would provide the appropriate level of care. They continually make rounds on the floors to make sure that discharges occur in the appropriate time period and to ensure that environmental services turn rooms around quickly and efficiently.
Initially, the PPCs managed to decrease the overall length of stay by one day within the medical division. In time, the surgical division was added to the PPCs' expanding area of coverage. This led to holding "Bed Briefings" twice a day. These forums involve all of the head or charge nurses from each floor and unit and are led by the PPCs. During these mandatory 20-minute meetings, all active and potential discharges, admissions, transfers (internal and external), bed reservations, and logistics issues are identified and reviewed. The PPCs act as the negotiators in resolving and/or clarifying the true bed needs of the patients and often discuss case specifics with the admitting physicians. At any given time, the PPCs know the exact number of open beds for every floor and unit as well as specific needs for all admissions. The PPC originally operated during daytime hours only, Monday through Friday, but due to their extreme success they have been expanded to a 24/7 operation.
For example, prior to the development of the PPC role, medical "mini-unit" patients were waiting an average of 54+ hours in the ED before being transferred to a mini-unit setting; now the average time is less than 24 hours. The average waiting time in the recovery rooms dropped 60% in the first month after the PPCs began controlling the post-operative bed assignments in the Surgical Division.
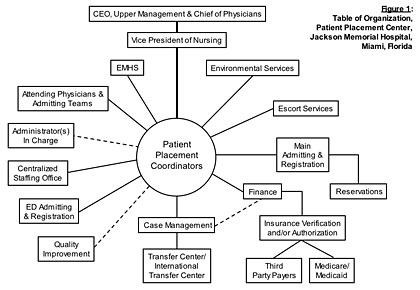
The PPCs' success in resolving bed assignments led the way to developing their own Patient Placement Center with administrative authority and strong administrative support over ancillary services such as escort services, environmental services, etc. (see Figure 1). As an adjunct to this new center, centralized staffing is coming under their auspices to better balance staffing availabilities and abilities with actual patient needs.
Emergency Medical Hospitalist Service
The second initiative to develop was the Emergency Medical Hospitalist Service (EMHS). The goals of this service are to provide attending-level care to patients requiring admission, allow the hospital to operate within the admission cap guidelines set forth by the RRC, and to function during the time in which the ACGME work hour limits were affecting the hospital. Two internists were hired to admit patients overnight and begin their medically necessary inpatient work-ups.
During each shift, EMHS admits and initiates the inpatient care of all medical admissions for inpatient services. During a typical 12-hour shift (8 pm to 8 am), EMHS admits an average of 10 to 12 new patients from the ED. As soon as the ED physician makes the decision to admit the patient, one of the hospitalists interviews, examines, and writes admission orders on the patient. Their presence speeds up the process of the patient's evaluation and allows the patient to be immediately transferred to an assigned in-house bed, thus expediting the patients out of the chaotic ED environment. This also allows the admitting physician to develop a rapport with the patient in the middle of the night, instead of feeling rushed in the morning to round on as many as 20 new patients. Understandably this assures a better night's rest for the patient and improves the institution's bed utilization. Moving patients to the floor in a timely fashion also allows for the ED to treat more patients in a safer and more appropriate manner. Toward the end of the shift, the newly admitted EMHS patients are signed out to the appropriate medical teams.
The evening and nighttime PPCs also serve as liaisons for the EMHS physicians whenever nursing-related issues arise within the various treatment areas. To further facilitate direct communication between these two services, cellular telephones with two-way radio capability were assigned to each of the PPCs and EMHS physicians. Later a "fast-track" system was developed with the PPCs and escort services to move the admitted patients more rapidly to appropriately assigned beds.
Since the two roles were instituted, there have been notable improvements in the ED's throughput, inpatient bed utilization, patient satisfaction, decreased average length of stay (both in the ED and inpatient), and improved quality of care.
To improve the movement of telemetry bed availabilities, ARNPs assigned to the cardiology teams developed a protocol. This protocol, along with physician-approved algorithms, allows the ARNPs to discontinue telemetry monitoring thus opening up more telemetry beds for newly admitted patients waiting in the ED. With this initiative in place, telemetry beds became available 50% faster than prior to this established practice. This in turn helps to decompress the number of telemetry patients waiting in the ED.
One of the latest efforts brought forward has been "SWAT Team Discharging" jointly initiated by the social services and case management departments. The institution is also reviewing automated systems to interface with existing computerized systems to enhance data collection and facilitate patient movement even further.
Indeed, developing these programs has been a challenge and even newer challenges lie ahead. However, once the hospital's administration saw the improvements and increased productivity, they began expanding the staffing and the services for both groups.
Aman Sabharwal is an emergency medicine hospitalist (nocturnist) at the University of Miami/Jackson Memorial Hospital. He is a 2000 graduate from the University of Missouri School of Medicine, completed his internal medicine residency at the University of Miami/Jackson Memorial Hospital, and is board certified in internal medicine. During the last year of his residency, he helped to design the Emergency Medicine Hospitalist Service and was instrumental in the development of the hospital's nocturnist service. He also serves as an attending physician for the inpatient teaching services and is involved in quality assurance and utilization projects.
Roshan K. Rao is an emergency medicine hospitalist (nocturnist) at the University of Miami/Jackson Memorial Hospital. He is a 2000 graduate of the University of Tennessee — Memphis — School of Medicine, a graduate of Oberlin University, and completed his residency at the University of Miami/Jackson Memorial Hospital. He is also board-certified in internal medicine and his current areas of research include cardiac and renal diseases/disorders. He also helped to develop the Emergency Medical Hospitalist Service and serves as an in-patient teaching attending.
Janice K.Gonzalez is the administrator of the Patient Placement Center at the University of Miami/Jackson Memorial Hospital. She is a 1982 graduate of the former Jackson School of Nursing and has worked at Jackson Memorial for 22 years as an in-patient head nurse, a case manager for trauma services and as a trauma nurse specialist within the emergency department.
Mitchell G. Mason is a patient placement coordinator at the University of Miami/Jackson Memorial Hospital. He is a 1985 graduate of Hocking College School of Nursing in Nelsonville, Ohio, and a 1981 graduate of Ohio University's College of Education. For 17 years, he worked in the emergency department as a trauma nurse specialist, assistant nurse manager, and clinical resource coordinator. Mason has authored several other publications and freelances as a professional consultant/expert witness for various attorneys throughout Florida.
|
 |
 |
 |




















|
 |

