Case Study: Improving Medication Safety with a Wireless, Mobile Barcode System in a Community Hospital
May / June 2005
Case Study
Improving Medication Safety with a Wireless, Mobile Barcode System in a Community Hospital
Over the past few years, hospital organizations have increasingly looked to new technology solutions to improve patient safety. Barcode technology is an especially promising approach in the effort to reduce medical errors. While barcode technology has been used for quite some time in many hospital applications, it has only recently been used to address patient safety. The use of barcode technology at the patient’s bedside has shown impressive gains in reducing medication administration errors, which may account for as many as 7,000 deaths per year in U.S. hospitals (IOM, 2000).
Barcodes provide a valuable verification of medication administration by assuring that the “five rights” are confirmed — right patient, right medication, right dose, right time, and right route of administration. While studies conducted in VA hospitals in the early 1990s showed that the use of barcodes reduced medication administration error rates by up to 86% (Meadows, 2003), community hospitals are just beginning to use this technology to improve patient safety. Recent estimates indicate that only 2% to 6% of hospitals are currently using barcodes to reduce medication administration errors (Center for Business Innovation, 2004).
Background
This case study examines the use of a wireless, mobile barcode medication administration system at Beloit Memorial Hospital in Beloit, Wisconsin, a 175-bed community hospital with four off-site clinics, serving a population of approximately 175,000 residents living in southwestern Wisconsin and northwestern Illinois.
The hospital has a formal affiliation with the University of Wisconsin Hospital System and an active though informal affiliation with Rockford Hospital in Rockford, Illinois. The hospital’s Board of Trustees, composed of 10 medical professionals and community leaders, has committed the hospital to a primary goal of providing high-quality healthcare services for all patients.
In September 2003, Beloit Memorial installed a wireless, handheld barcode medication administration system in its Family Care Center (FCC) unit, consisting of 35 ob/gyn, pediatric, and labor/delivery beds. This pilot resulted in a 67% decrease in medication administration errors within the first four months of operation. With the pilot successfully completed, the hospital expanded implementation of the barcode system to four additional inpatient units. This case study documents Beloit’s experience in these units, which included:
- Special Care Center (SCC) Oncology
- Multi Care Center (MCC) General Medical Surgical
- Intermediate Care Center (ICC) Telemetry
- Critical Care Center (CCC) Critical Care
These units presented a more complex environment than the FCC, treating patients with generally more serious medical conditions, who often required more medications. Consequently, these units were more prone to experience medication administration errors.
Goals and Objectives
The main goal of this study was to identify and measure the benefits of a wireless barcode system to reduce medication administration errors.
To address this goal the following specific objectives were established:
- Conduct an onsite visit, both pre- and post-implementation of the wireless barcode system in the four new inpatient units.
- Determine pre- and post-implementation medication administration error rates in these units.
Methodology
Pre- and post-implementation site visits were conducted by an independent consultant who interviewed senior nursing management, the unit managers, and the nurses charged with medication administration responsibilities; and observed the medication administration rounds.
The pre-implementation visit was conducted in late June 2004, and the post-implementation visit was conducted in December 2004, to review the results of the system four months after the “go-live” date. This interval was selected to ensure that the nursing staff was familiar with the barcode system and had completed its learning curve of the new system.
Patient Safety Goals
The hospital Board of Trustees and senior management have focused on establishing a culture of cooperation and communication aimed at improving the quality of patient care. This culture was key to embarking on a successful patient safety program. While the hospital established a Patient Safety Committee in 2001, the barcoding initiative originated from a recommendation by the director of pharmacy, who felt that additional checks and safeguards at the point of medication administration would be valuable in reducing medical errors. As a result, the hospital embarked on its initial barcode pilot in September 2003. The alignment of the board and senior hospital management including the CEO, the vice president of nursing, and department heads created a positive atmosphere and communicated a clear, unified message from senior management that led to the adoption and funding of the new barcode system.
Anticipated Benefits
In expanding the use of barcode technology to the additional inpatient units, the hospital hoped to achieve the following benefits:
- Improve patient safety through the reduction of medication administration errors, while minimally increasing nurse staffing time requirements.
- Improve nursing staff job satisfaction.
- Improve patient satisfaction.
- Generate positive public relations with the local community.
Barcode Implementation at Beloit
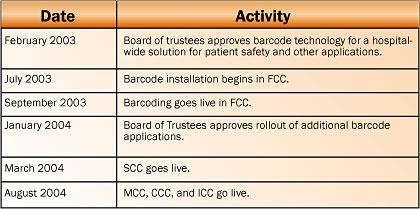
In February 2003, the Board of Trustees unanimously approved funding for a bar-code pilot project in the FCC, which began in July 2003. By January of the following year, the hospital approved the further deployment of barcoding for medication administration to include four additional inpatient units due to the FCC’s early success. Implementation of the original pilot and subsequent rollout to the other inpatient units occurred over a 15-month period from July 2003 through October 2004. The SCC went live in March 2004. The MCC, CCC, and ICC all went live in August 2004. This chronology is shown in Figure 1 below.
![]()
Staff Training
The SCC, an oncology unit, was selected as the second unit for barcode utilization implementation due to the fact that it administered many medications yet it was a relatively small unit with seven beds.
SCC staff training on the barcode system was conducted over a one-week period immediately prior to go-live. The training was conducted by “super users,” FCC nurses experienced and proficient with the system. These super users volunteered to assist in the SCC training. In addition, training staff from the vendor were on site to assist with the 4-hour training sessions, in which all 12 unit nurses were trained.
Once the staff training was completed, barcoding went live in March 2004. Daily meetings were held with the nursing staff during the first two weeks following implementation to troubleshoot any problems and to provide rapid response to questions about the system. In addition, a dedicated notebook was placed in the SCC where nurses could write comments, provide feedback, and ask questions about the system. The notebook was reviewed regularly by nursing managers to address issues quickly. In addition, daily management meetings were conducted with the director of pharmacy, director of IT, and the nurse unit manager to ensure that the system was working properly. The implementation proceeded smoothly, and hospital management reported that they were extremely satisfied with the system.
Based on the success of the implementation in both the FCC and the SCC units, the decision was made to bring on three additional units simultaneously. A training design similar to that used in the SCC was implemented using super users as well as on-site support from the vendor. The MCC, CCU, and ICC went live in August 2003.
A total of approximately 100 nurses were trained for these units. Training was conducted 48 hours prior to go-live. Eight super users were utilized in the training and were present on the units during the implementation. Going forward, new staff will be trained exclusively by the super users, eliminating the need for ongoing training by the vendor and reducing costs.
Hospital management was extremely pleased with this training approach. This can be attributed to several factors including careful, advance planning, continual communication with nursing staff both prior to and following implementation, a flexible training schedule to accommodate all shifts, and the fact that the barcode utilization process had been carefully integrated into the medication administration workflow processes.
Other factors also had a positive influence on the barcode system adoption in these new units including the initial success of the FCC pilot and nursing staff’s generally high level of satisfaction with the new system. These factors were publicized both formally by hospital management and, perhaps of equal importance, were communicated informally by staff nurses throughout the hospital.
|
Components of Wireless Barcode System |
Implementation Challenges and Solutions
Implementing a new system like barcode medication administration can present many challenges as nursing staff adapt to new work processes. Beloit Memorial encountered few objections by the nursing staff, though a few minor concerns were expressed about “having to learn new technology.”
Implementing the system in the Critical Care Center was somewhat more challenging. Initial concerns were expressed regarding the need to administer some drugs on an emergency basis or administering drugs to newborns within one hour after birth to comply with state law, and the new system changed work processes in a manner that they felt could potentially compromise patient care. The commitment to safe patient care was reinforced by management as the key treatment goal that would take precedence over the use of the barcode system in emergency situations.
Once the system was installed and the CCC staff became more familiar with the new system, these concerns did not resurface. Further, several staff were personally involved in situations where the system stopped a medication error from occurring, successfully demonstrating that their patient’s safety had been enhanced through the use of the wireless, barcode medication administration system.
Another issue that needed to be addressed during the implementation was the lack of barcodes on some of the unit-dose drugs being used. The barcodes had not been affixed to some unit dose medications, as required, due to a temporary staffing shortage in the pharmacy. This issue was quickly resolved and did not reoccur. However, this does suggest that the hospital pharmacy must be intimately involved in the planning and implementation of any new barcode utilization system for medication administration. The pharmacy department needs to consider the additional time that will be required to affix medications with barcodes.
Despite the implementation of the new barcode system and the changes in work processes that it necessitated, the hospital was not required to hire additional pharmacy or nursing staff.
Benefits Realized: Patient Safety Improvements
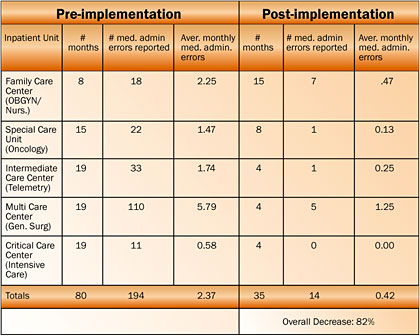
A comparison of the medication administration error rates pre- and post-implementation shows that medication administration errors were reduced by an average of 82% for the five units studied (see Figure 2).
![]()
The post-implementation data was collected from the go-live month in each unit through November 30, 2004, the most recent data available at the time of this study. The reported post-implementation time periods ranged from 4 to 15 months experience, depending on the unit. This data includes the first month that the system was installed, when staff learning curves were steepest and errors were most prone to occur. If the first month of implementation is not included, to allow time for learning the new system, the medication administration error rate is decreased even further to an average of 93%.
All participating units reported significant error reduction with the greatest numeric decline in monthly average medication errors occurring in the MCC, which fell from an average of 5.8 to 1.25 medication errors per month. The error rate in this unit was high in comparison to the other units because the MCC is the largest unit with a total of 64 licensed beds.
The types of medication errors that occurred in these units varied and included instances of wrong dosage, missed medication, missed drug reaction, or wrong IV bag hung and were documented in the hospital’s Med Event Report.
Other Benefits Realized
The benefits of the barcode system extend beyond a decrease in medication administration errors. They include:
Improved nursing staff satisfaction. Increased job satisfaction was identified as an additional benefit of the system. The nursing staff felt that the hospital was truly committed to improve quality of care by investing in state-of-the-art technology to improve patient safety. Recruitment of new staff was also mentioned as an additional potential benefit. Showing the hospital’s advanced use of technology was cited as a positive factor in recruiting new staff in a competitive employment environment.
Patient satisfaction. During the initial implementation, all patients were briefed about the new medication administration system and why it was being installed. Nurses reported a genuine sense of appreciation from patients and their families that the hospital was committed to patient safety, as demonstrated by use of the new system.
Improved community relations. After deciding to implement a new medication administration system, the hospital contacted the local media and sent senior management to speak with local citizen groups (e.g., Rotary International) to educate the community about the new system and why it was being implemented. This public relations exposure helped to build on the existing positive relations between the hospital and the local community and resulted in several stories in the local press.
Future Automation Directions
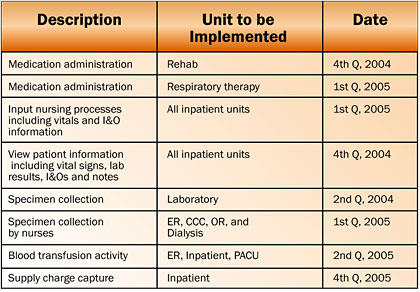
Currently, the hospital is committed to proceeding with the rollout to make full use of other wireless mobile barcode applications. The rehab unit went live in the fourth quarter, 2004. It is expected that wireless barcoding will be implemented for respiratory therapy by the first quarter, 2005. Other barcode applications will also be installed at the hospital in accordance with the implementation schedule shown in Figure 3.
![]()
Conclusion
Recent reports indicate that five years after the Institute of Medicine’s landmark study, To Err Is Human: Building a Safer Health System (2000), hospitals have made little progress in implementing patient safety solutions to reduce medical errors. This case study has documented the experiences of one community hospital, committed to a culture of patient safety, which has demonstrated the success of a wireless mobile barcode system. This resulted in a reduction of medication administration errors, in the inpatient units observed, by an average of 82% after being installed for a relatively brief period of time (5 to 15 months).
Additional benefits attributed to the barcode system were also identified. These include improved staff and patient satisfaction, and generation of positive press and public relations with the local community.
In the final analysis, success of the barcode medication administration system at Beloit Memorial can be attributed to not only the use of state-of-the-art technology, but also to a carefully constructed, fully communicated work plan that included clearly identified new work processes and a thorough staff orientation and training program.
References
Institute of Medicine (IOM). (2000). To err is human: Building a safer health system. L. T. Kohn, J. M. Corrigan, & M. S. Donaldson (Eds.). Washington, DC: National Academy Press.
Meadows, M. (2003). Strategies to reduce medication errors, FDA Consumer 37 (3).
The Center for Business Innovation. (2004, November 18-19). The evolution of bar coding and patient safety: Update 2004, The third annual summit on patient safety and information technology (panel discussion).
Work, M. (2004). Demonstrating benefits in a community hospital through the use of wireless, mobile barcode technology in medication administration: A case study. Retrieved April 21, 2005, at www.carefusion.com/includes/CaseStudies.asp
