Viewpoint: HHS’ $840 Million Gamble
As a follow-up to PfP and HEN, TCPI represents another of HHS’ healthcare improvement efforts to deploy proven practices with a focus on enhancing IT infrastructure and data systems. Among the organizations chosen to be PTNs is the American Medical Association (AMA), the largest trade association of physicians in the United States. However, the AMA is exempted from any direct recruitment of physicians whatsoever—curious, given that the AMA’s membership is the largest of any physician group in the United States.
Physician burnout
Governmental efforts to “transform” clinical practice (through the use of electronic health records, interoperable data systems and IT infrastructure, peer-learning networks, patient-centered care, and person and family engagements) are challenged by the stark revelation that physicians are burning out (defined as emotional and physical exhaustion) at an alarming rate. In fact, the proportion of physicians reporting burnout is higher than any profession in the United States, as reported by Shanafelt et al. (2012) in the latest installment of their research on physician work satisfaction: “Compared with a probability-based sample of 3,442 working U.S. adults, physicians were more likely to have symptoms of burnout (37.9% vs 27.8%) and to be dissatisfied with work-life balance (40.2% vs 23.2%).”
The AMA’s 2013 study conducted in collaboration with RAND Corporation identified electronic health records (EHR) as an emerging contributory factor to physician burnout: “In the practices we studied, physicians approved of EHRs in concept … However, for many physicians, the current state of EHR technology significantly worsened professional satisfaction in multiple ways. Poor EHR usability, time-consuming data entry, interference with face-to-face patient care, inefficient and less fulfilling work content, inability to exchange health information between EHR products, and degradation of clinical documentation were prominent sources of professional dissatisfaction” (Friedberg et al., 2013).
These findings (among others) led the AMA to launch its “STEPS Forward” initiative to offer strategies for dealing with burnout. In October 2015, at the 19th Management of the Hospitalized Patient program in California, Dr. Christine Sinsky, vice president of professional satisfaction at the AMA, noted that “70 to 80 percent of physician work output could be considered waste, defined as work that doesn’t need to be done and doesn’t add value to the patient” (Beresford, 2015).
Prior to the launch of TCPI, reports of physician burnout were eminent. In their authoritative study, Shanafelt et al. (2012) wrote that: “(1) the prevalence of burnout among US physicians is at an alarming level, (2) physicians in specialties at the front line of care access (emergency medicine, general internal medicine, and family medicine) are at greatest risk.”
Even without the issue of physician burnout, recruitment of physicians for nonclinical activities can be difficult. The survey conducted by Shanafelt et al. (2012) achieved a response rate of 26.7%. Data on the recruitment levels of PTNs and SANs for the first year are not publically available, but an overriding concern for the sponsors of TCPI should be the complaints from physicians about occupational burnout. These complaints should be taken seriously and addressed directly. 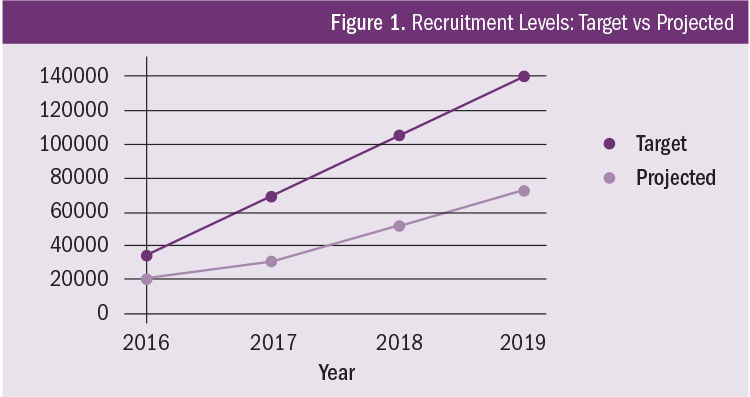
Physician engagement
The bold aims of TCPI must confront the reality of physician dissatisfaction with the current state of EHR technology. When considering the requirements of enrollment in PTNs and SANs, the likelihood of recruiting 140,000 physicians is uncertain. While some of the PTNs and SANs have met their physician recruitment goals (as reported at the 2016 CMS Quality Conference in Baltimore), many have not. At this rate, the overall recruitment goal may be difficult to attain (see Figure 1).
In the same way HHS has created a program to foster active engagement of patients and their families, the department should consider expanding provider and physician engagement protocols as a way to gain more buy-in from physicians. Considerations for the expansion of these protocols include: (1) automating data documentation and data reporting at the patient encounter level to reduce burden on providers, and (2) potential reimbursements for hiring specialists in health data documentation and data analysis to support clinical work.
Yoku Shaw-Taylor specializes in advanced analytics for healthcare improvement and process optimization and may be contacted at yshawt@hotmail.com.
References
Agency for Healthcare Research and Quality (2015). Saving lives and saving money: Hospital-acquired conditions update: Interim data from national efforts to make care safer, 2010–2014. Retrieved from https://www.ahrq.gov/sites/default/files/publications/files/interimhacrate2014_2.pdf
Beresford, L. (2015, October 23). AMA’s Christine Sinsky, MD, explains EHR’s contribution to physician burnout. The Hospitalist. Retrieved August 8, 2016, from www.the-hospitalist.org/article/amas-christine-sinsky-md-explains-ehrs-contribution-to-physician-burnout
Centers for Medicare and Medicaid Services (2016). Transforming Clinical Practice Initiative. Retrieved August 7, 2016, from https://innovation.cms.gov/initiatives/Transforming-Clinical-Practices
Friedberg, M. W., Chen, P. G., Van Busum, K. R., Aunon, F., Pham, C., Caloyeras, J. P., … Tutty, M. (2013). Factors affecting physician professional satisfaction and their implications for patient care, health systems, and health policy. Santa Monica, California: RAND Corporation.
Health Services Advisory Group & Mathematica Policy Research (2014, July 10). Project evaluation activity in support of Partnership for Patients: Task 2 evaluation progress report. Baltimore, Maryland: Center for Medicare and Medicaid Innovation.
Shanafelt, T. D., Boone, S., Tan, L., Dyrbye, L. N., Sotile, W., Satele, D., … Oreskovich, M. R. (2012). Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Archives of Internal Medicine, 172(18), 1377–1385.
