Perioperative Pressure Injuries: Protocols and Evidence-Based Programs for Reducing Risk
Extrinsic risk factors
- Duration of time immobilized before surgery
- Operation planned for three hours or longer
- Prone positioning
- Trauma
- Cardiac, orthopedic, vascular, transplant, or bariatric procedure
- Increased hypotensive episodes
- Use or continued use of vasopressors
- Reduced mobility on the first day postop
Additional risk factors have been correlated with pressure injury development outside the OR: current smoking history, dry skin, impaired mobility, altered mental status (i.e., confusion), urinary and fecal incontinence, malnutrition, physical restraints, malignancy, history of pressure injury, existing skin breakdown, and impaired sensation, as well as being bedbound, chairbound, or unable to reposition oneself (Lyder & Ayello, 2008; Minnesota Hospital Association, 2013).
Evaluating patients with risk assessment tools
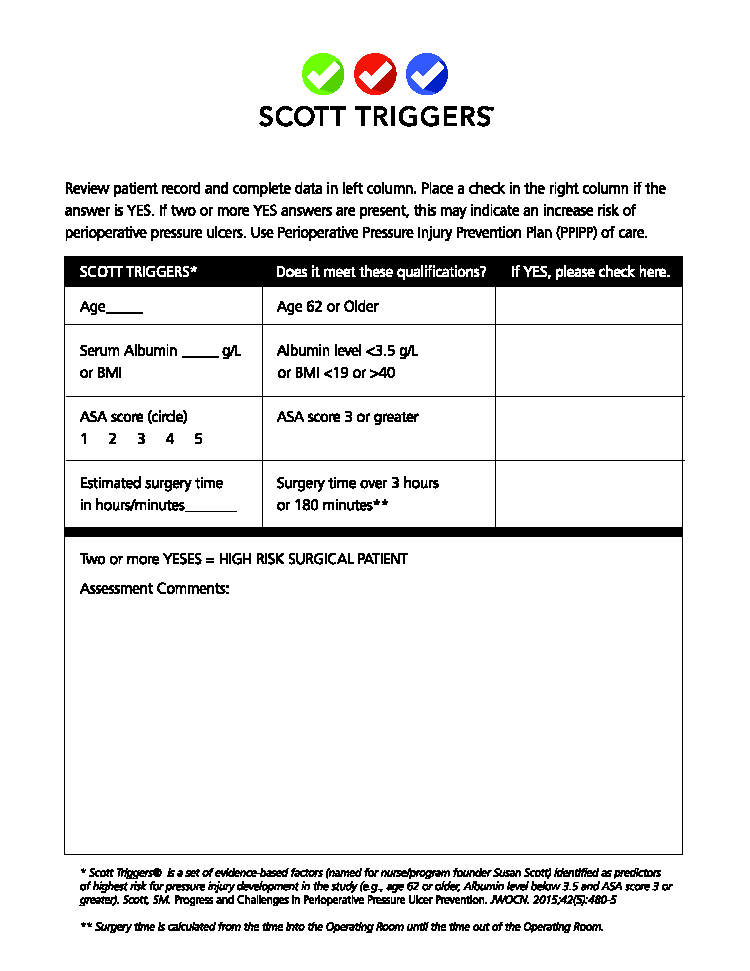
Several steps can be taken to decrease the incidence of pressure injury among surgical patients. They include understanding the epidemiology and presentation of pressure injury development, identifying patients at high risk, and assessing patients’ skin. These steps may require educating staff and physicians and familiarizing them with certain screening tools, such as the Scott Triggers Tool (Figure 1).
The Scott Triggers Tool identifies high-risk patients preoperatively by evaluating four evidence-based predictors of perioperative pressure injury—age, serum albumin or BMI, ASA physical status classification score, and estimated time of surgery. These nurse-designed, evidence-based predictors were identified in a study conducted at the VA Medical Center in Memphis, Tennessee (Scott, 2015). The tool prompts care providers to implement additional interventions to reduce the patient’s risk. It provides rapid, real-time identification of potential problems and enables timely, productive intervention at the patient level.
Other screening tools include the Munro Pressure Ulcer Risk Assessment Scale for Perioperative Patients (Munro, 2010) and the Braden Scale for Predicting Pressure Sore Risk (Braden, Bergstrom, & Ball, 2016). The Munro Scale is used to identify adult general surgery patients at risk for pressure injury development. It is not a skin assessment tool. The patient’s risk level is scored for each phase of surgery (pre-, intra-, and postoperative), and the cumulative score is communicated to the inpatient unit for continuation of care. The Braden Scale is used to evaluate a patient’s risk of developing a pressure injury by examining six criteria: sensory perception, moisture, activity, mobility, nutrition, and friction/shear. The total score can range from 6 to 23, with a lower score indicating a higher risk. The level of risk indicates the intervention strategies that should be used.
Implementing an OR skin bundle
Once a patient has been identified as being at high risk for developing a pressure injury, an OR skin bundle protocol should be implemented to mitigate harm. A bundle is a set of evidence-based interventions to help standardize care and reduce complications in the healthcare setting. Other successful evidence-based bundles include those for ventilator-acquired pneumonia and for central line infections (Waters et al., 2015).
An OR skin bundle may include the following interventions:
- Assessment of the patient’s skin preop and immediately postop
- Safe patient handling
- Standardization of high-specification* OR table pads
- Redistribution and offloading of pressure, particularly to heel and occiput
- Use of protective dressings
- Use of approved positioning devices
- Maintenance of normothermia and microclimate
- Handoff communication
- Postop:
- Early movement
- Daily skin assessment
- Pressure management
